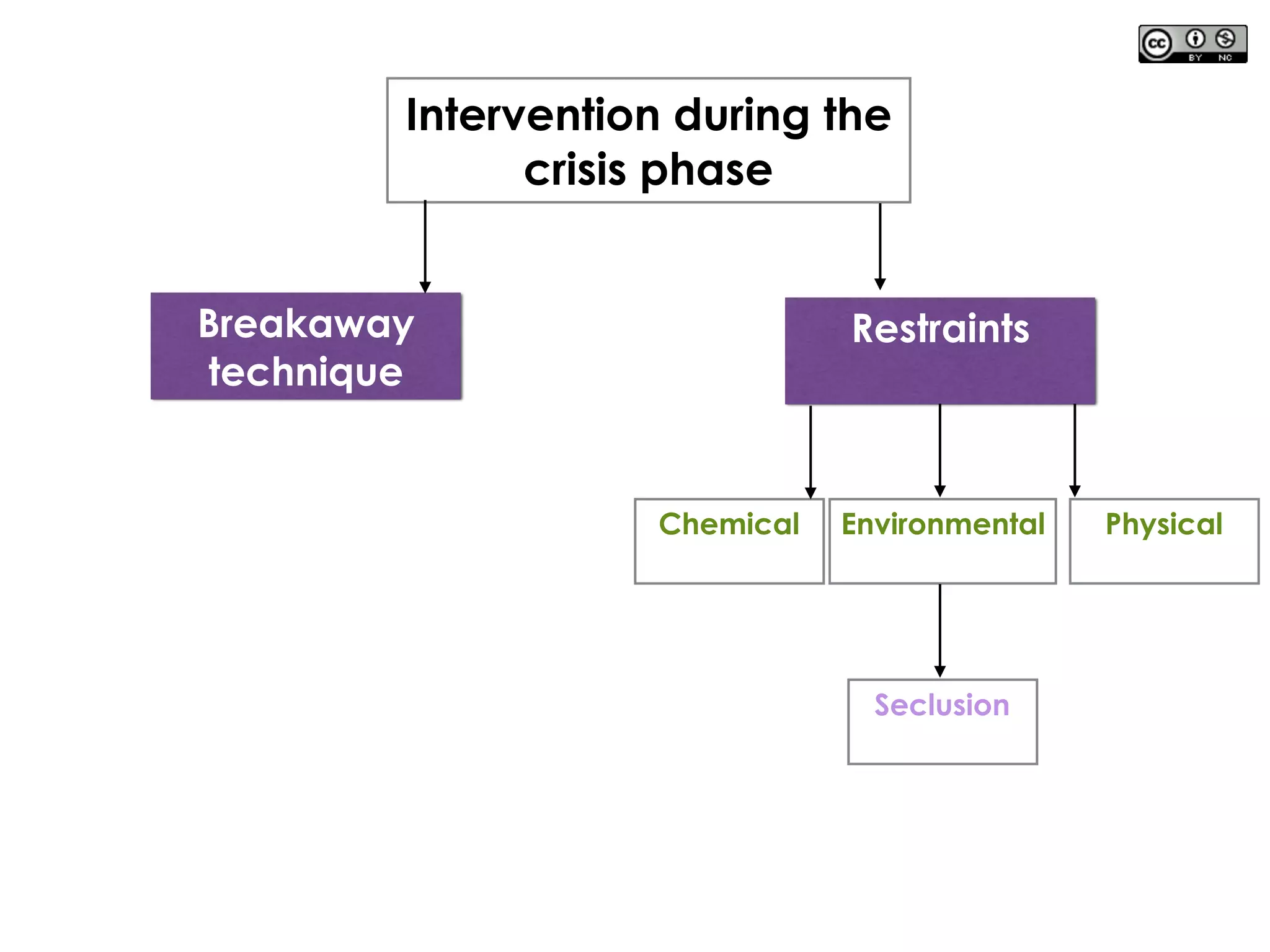
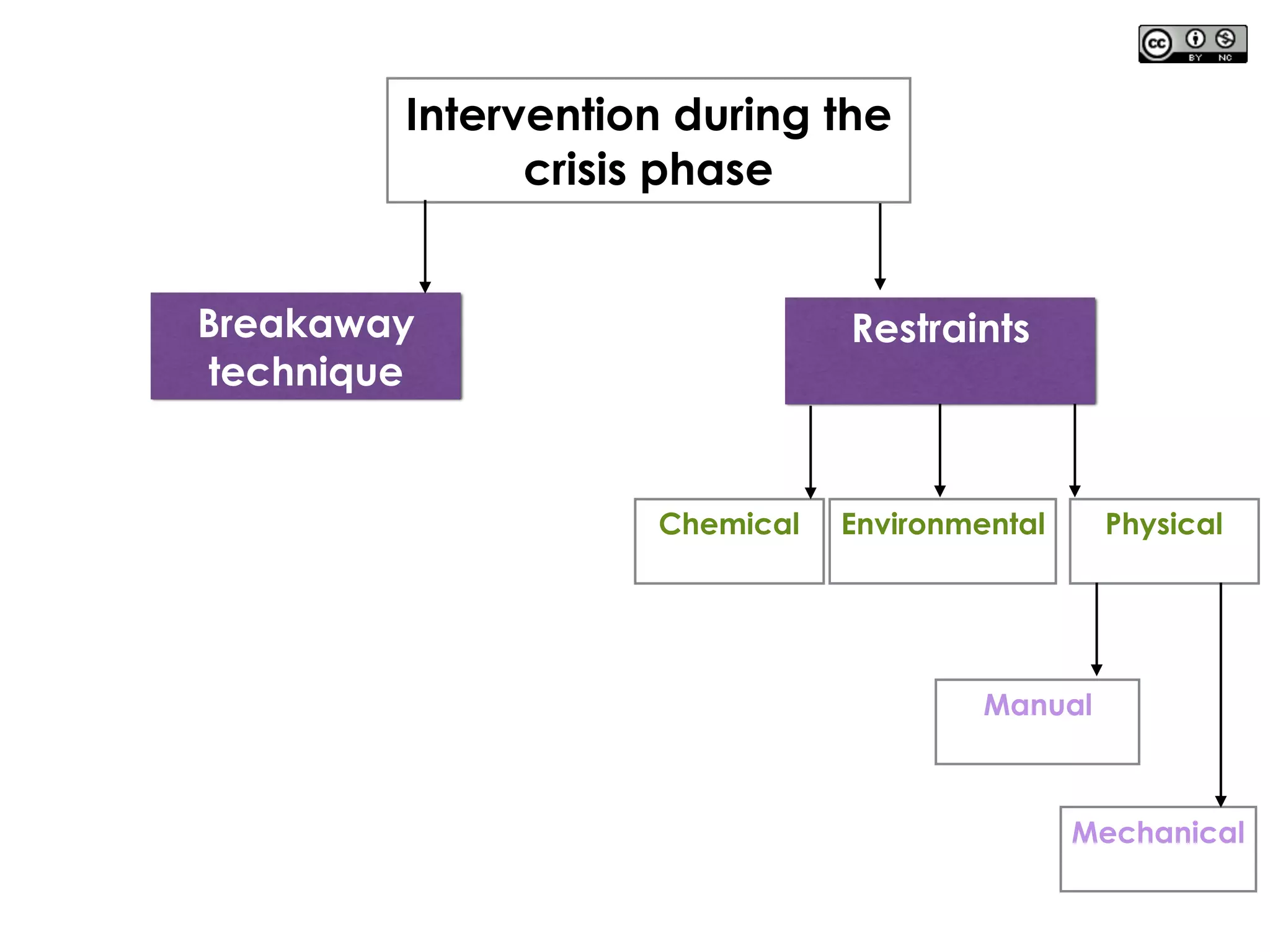
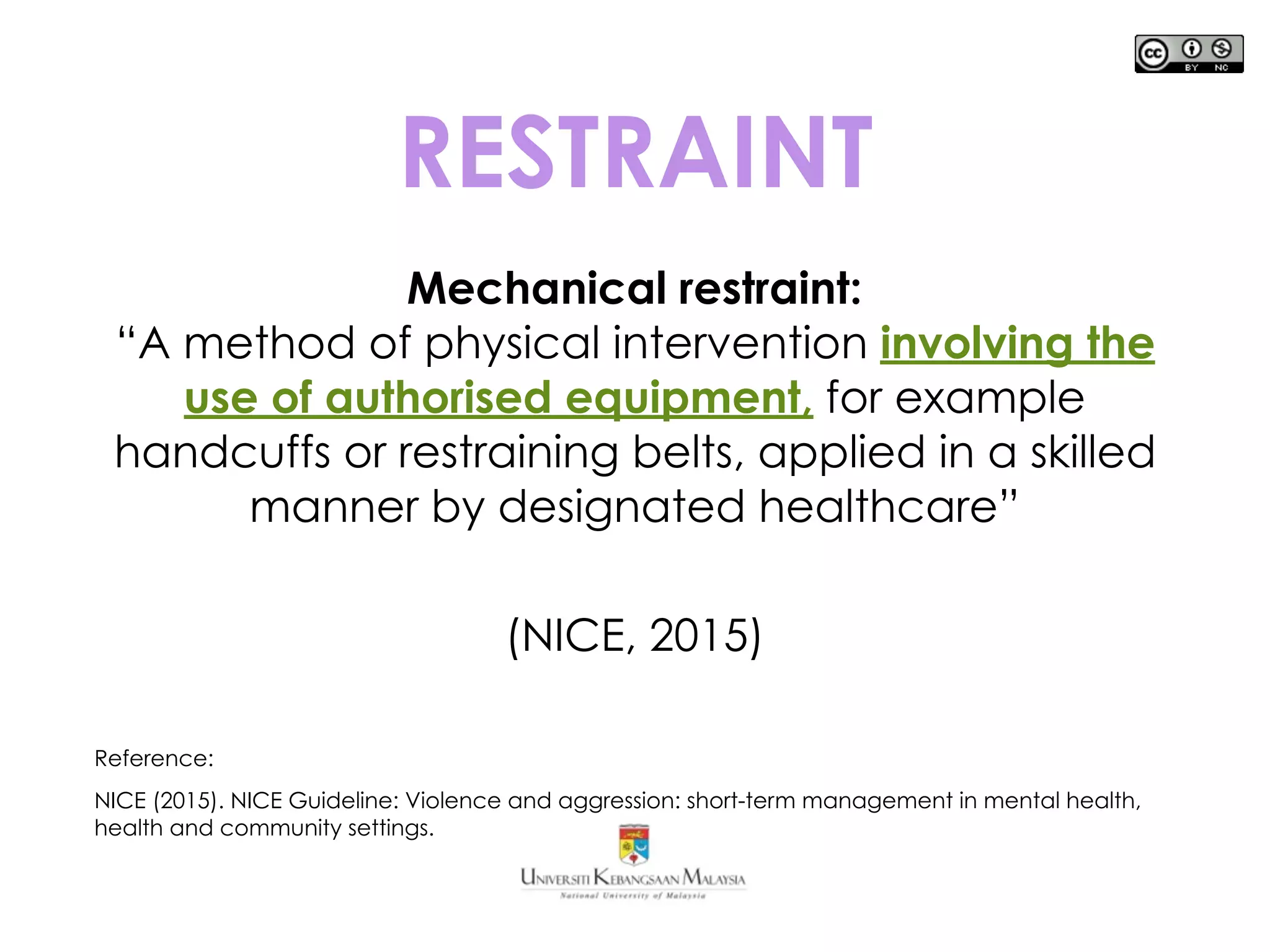
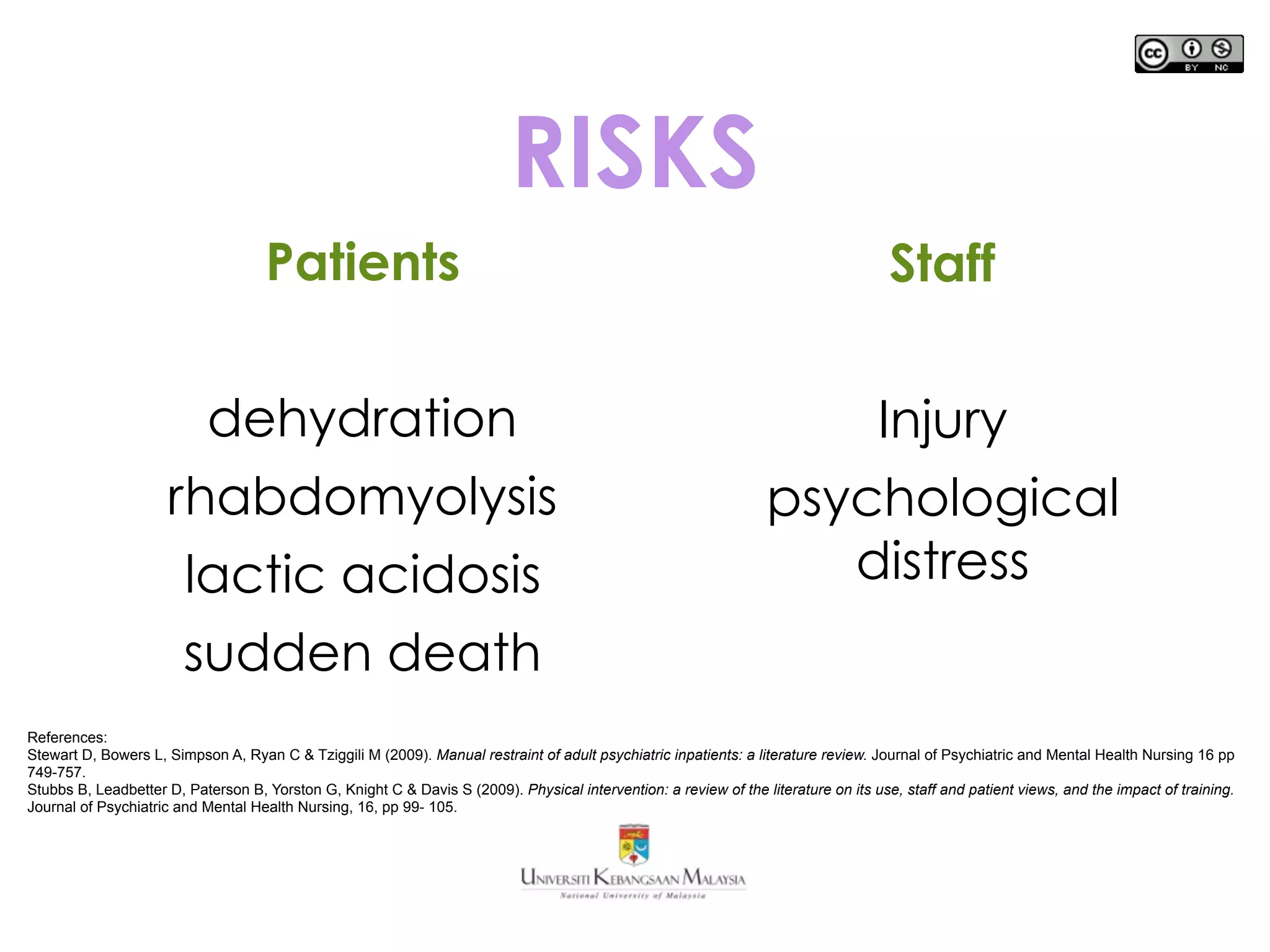
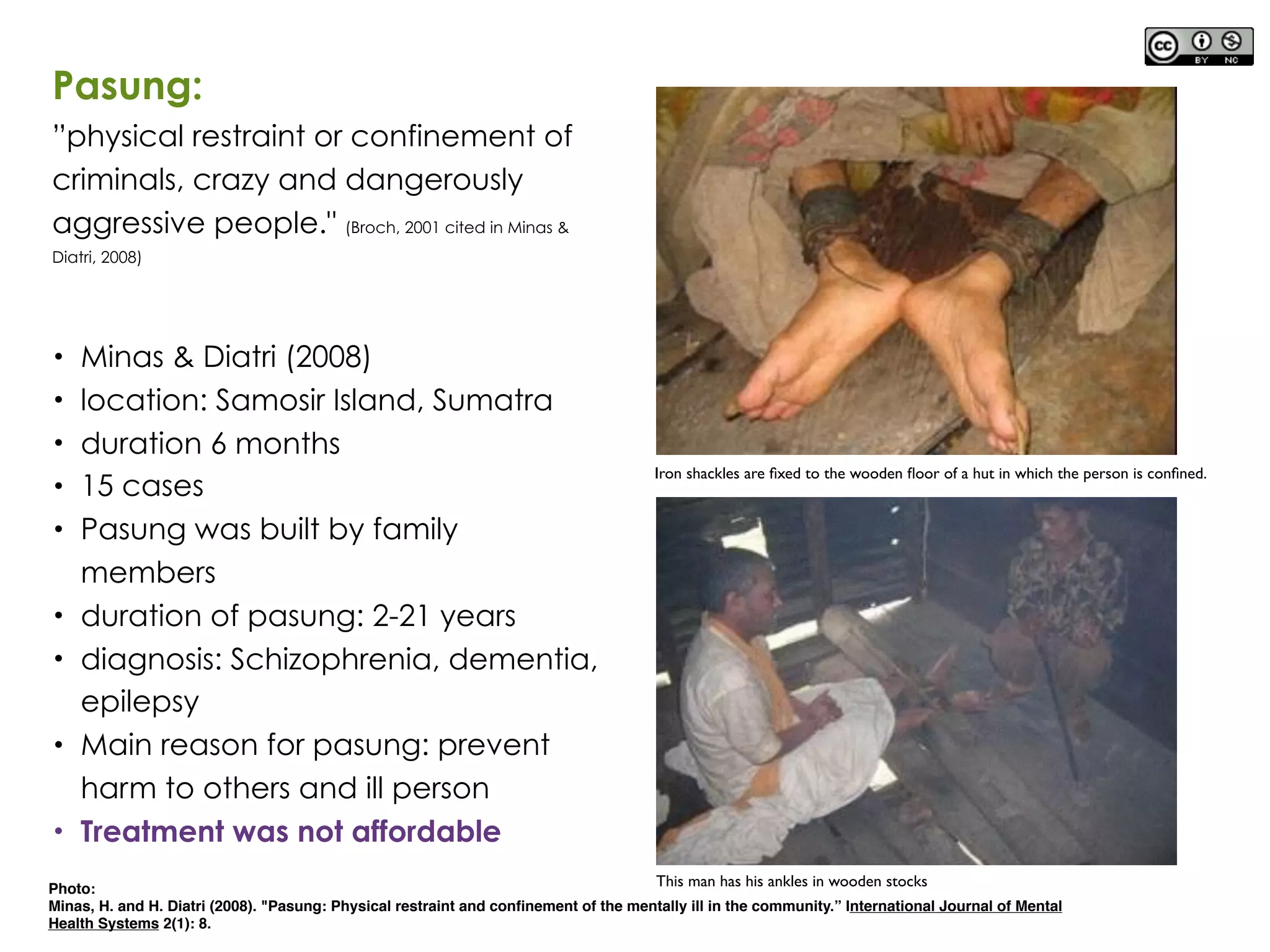
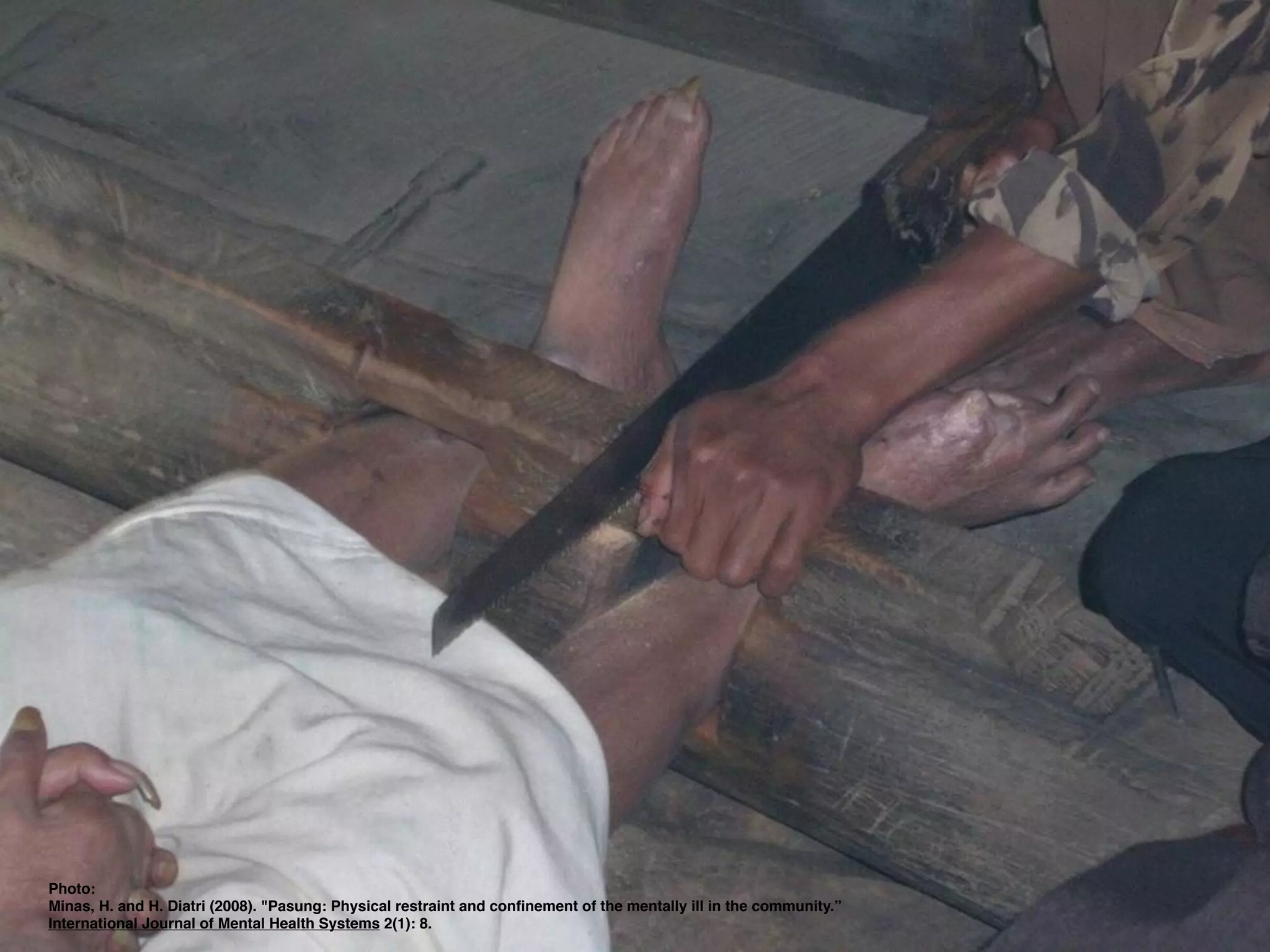
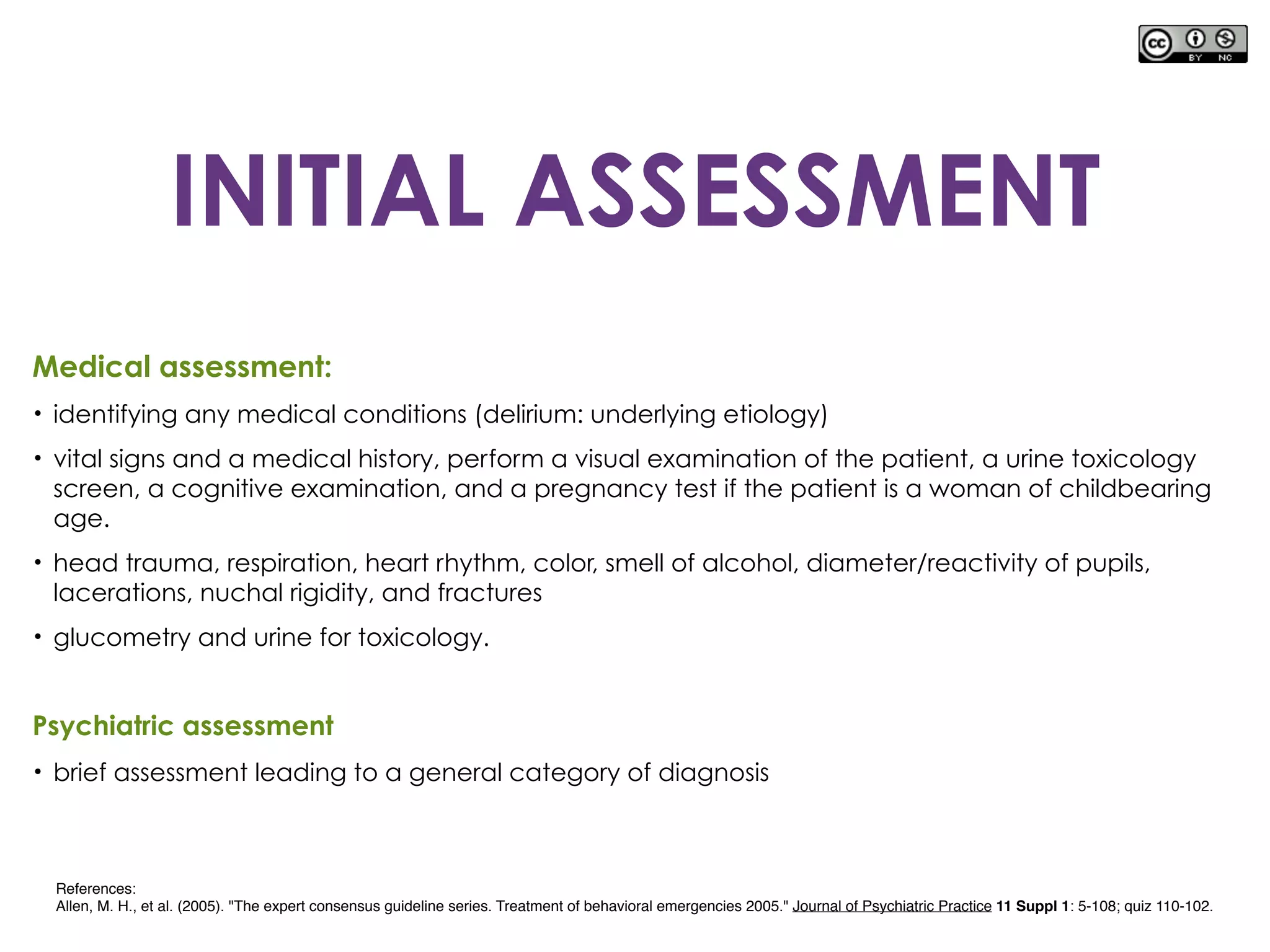
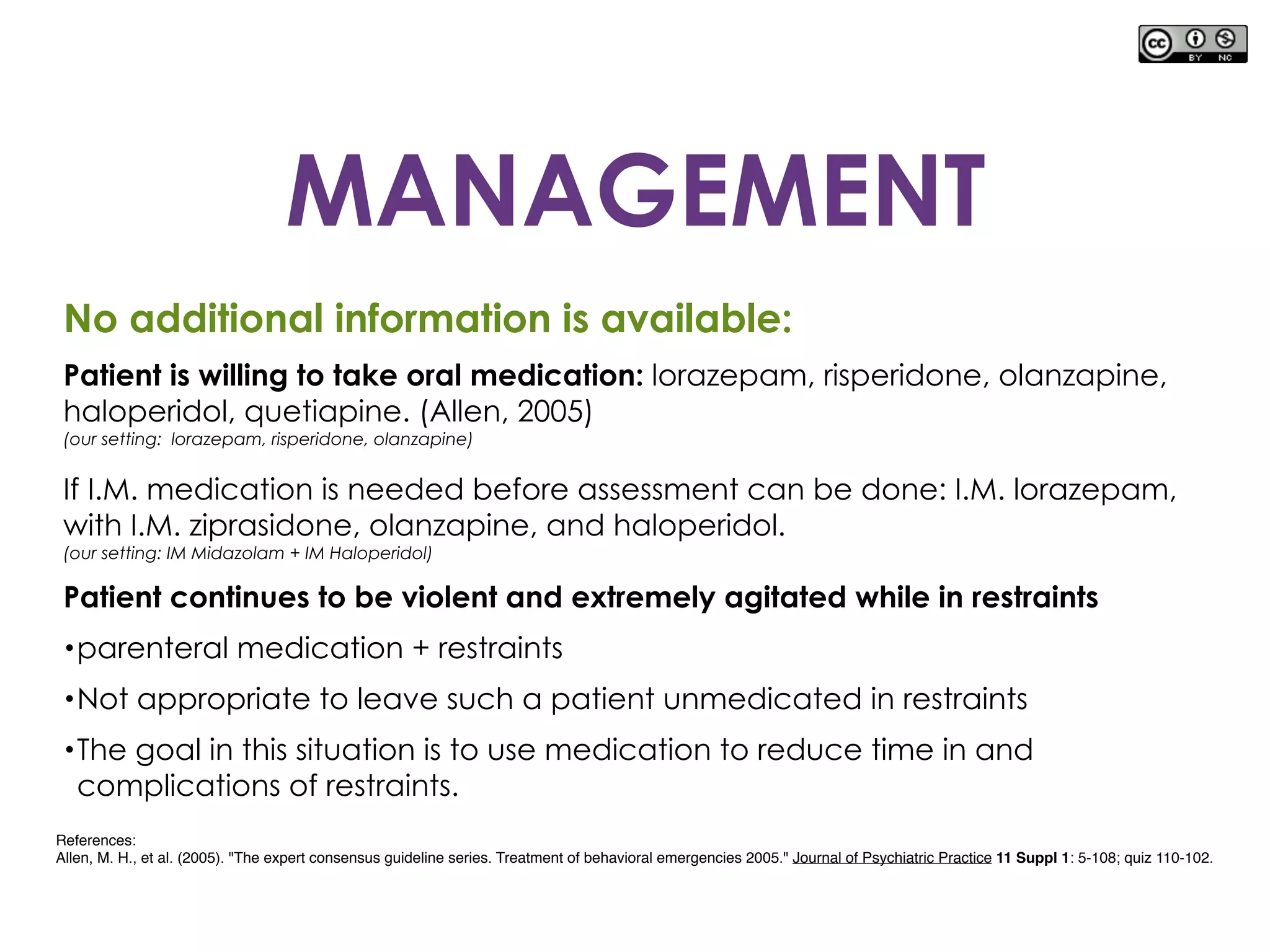
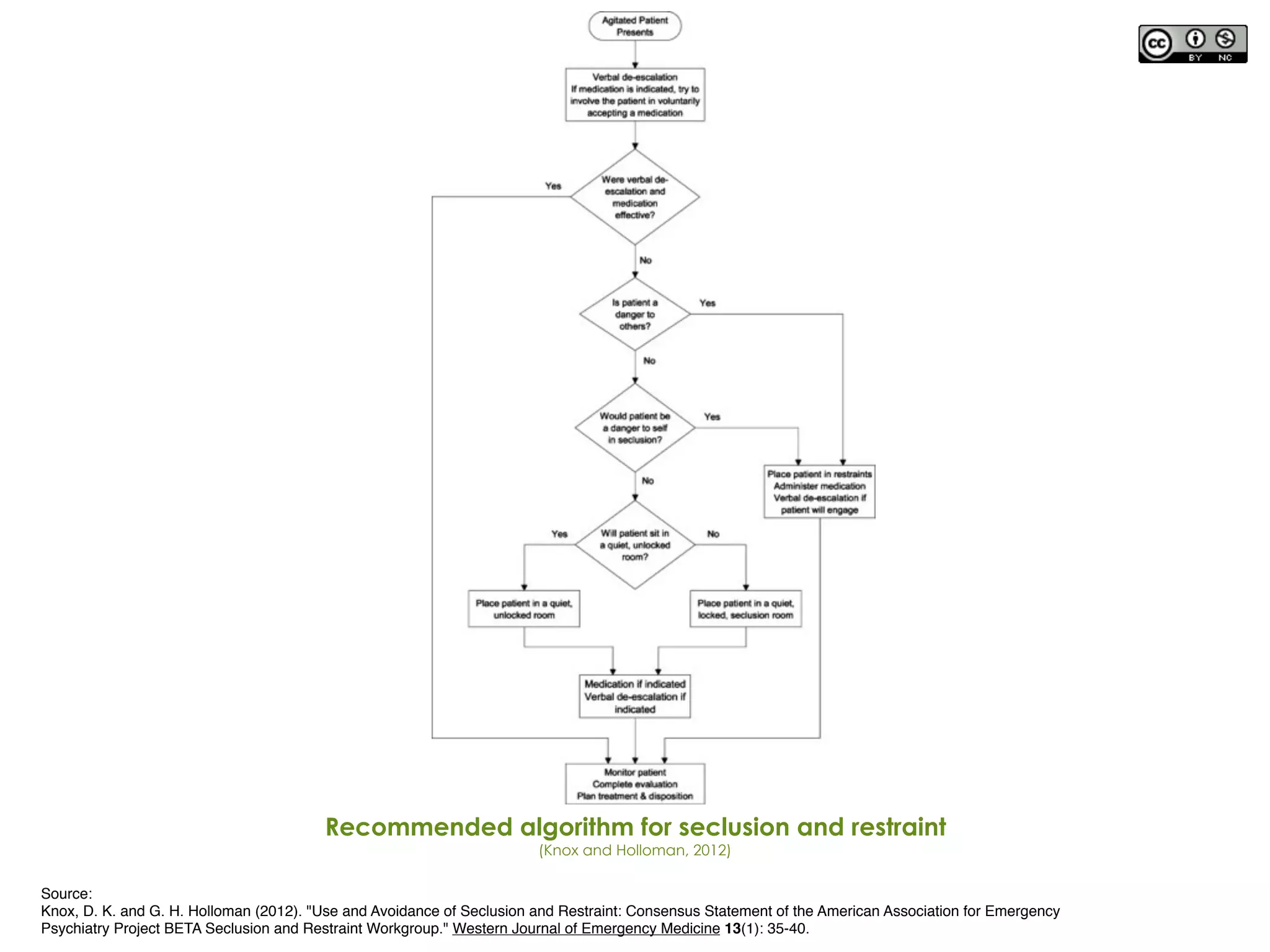
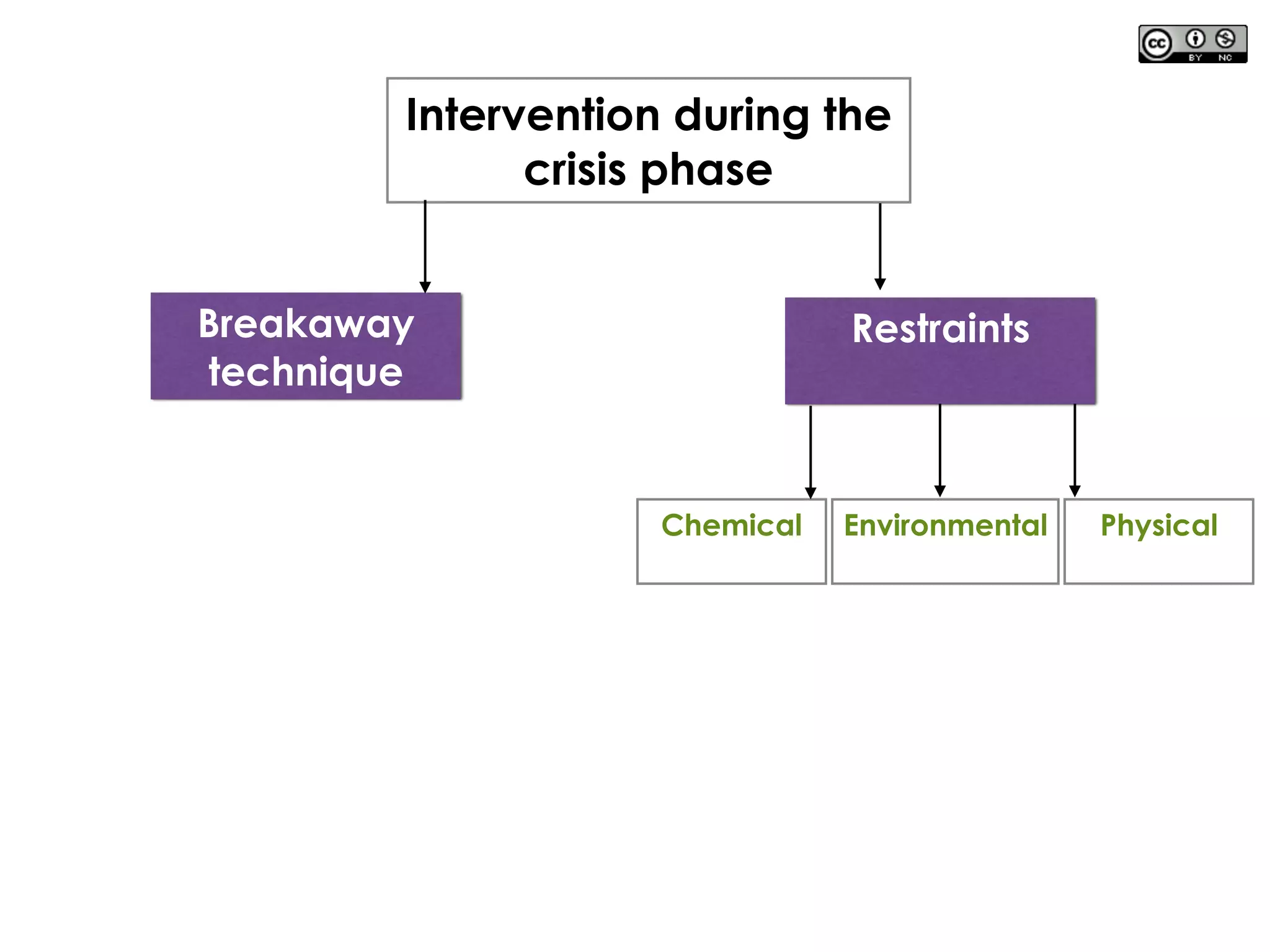
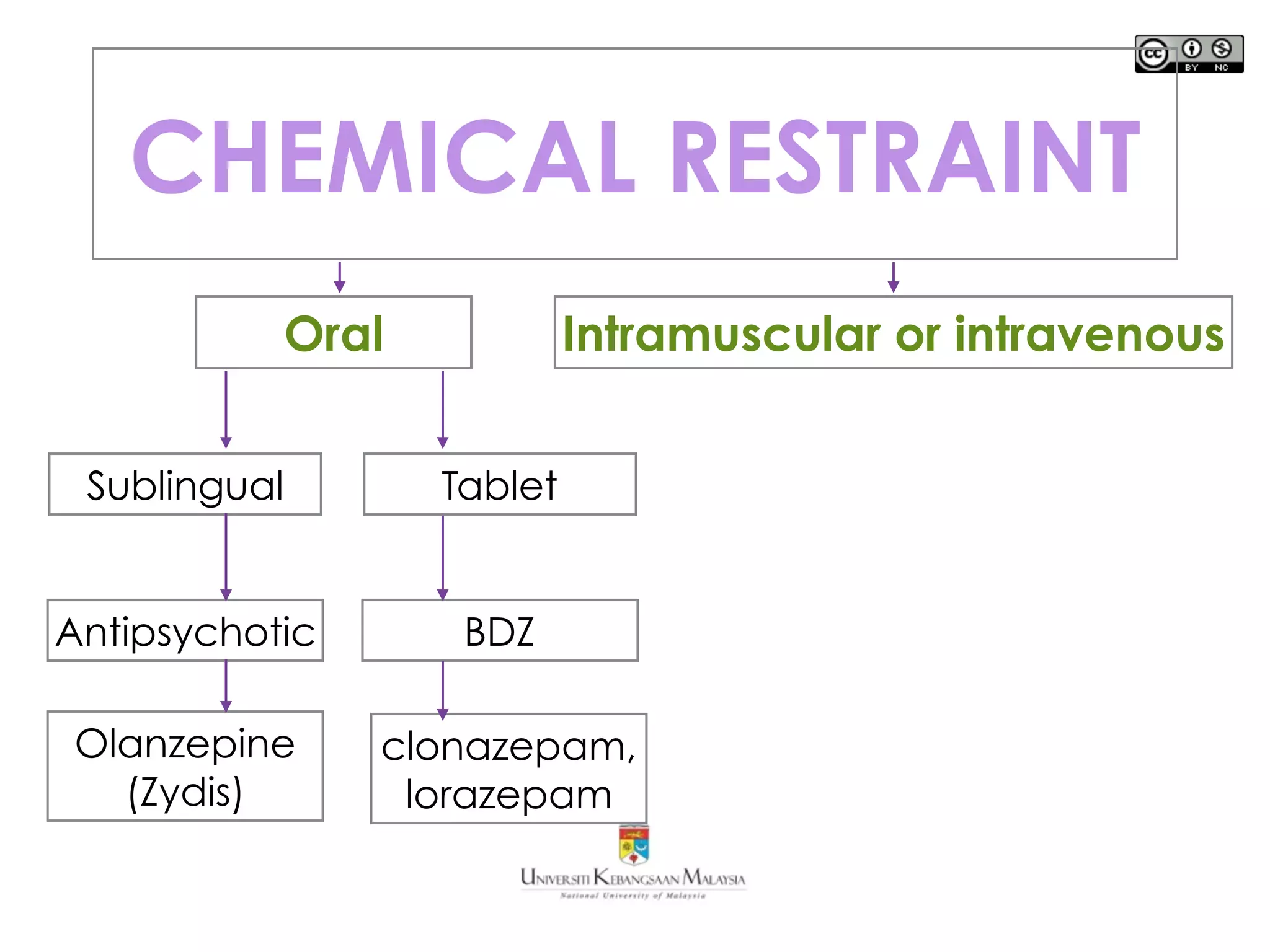
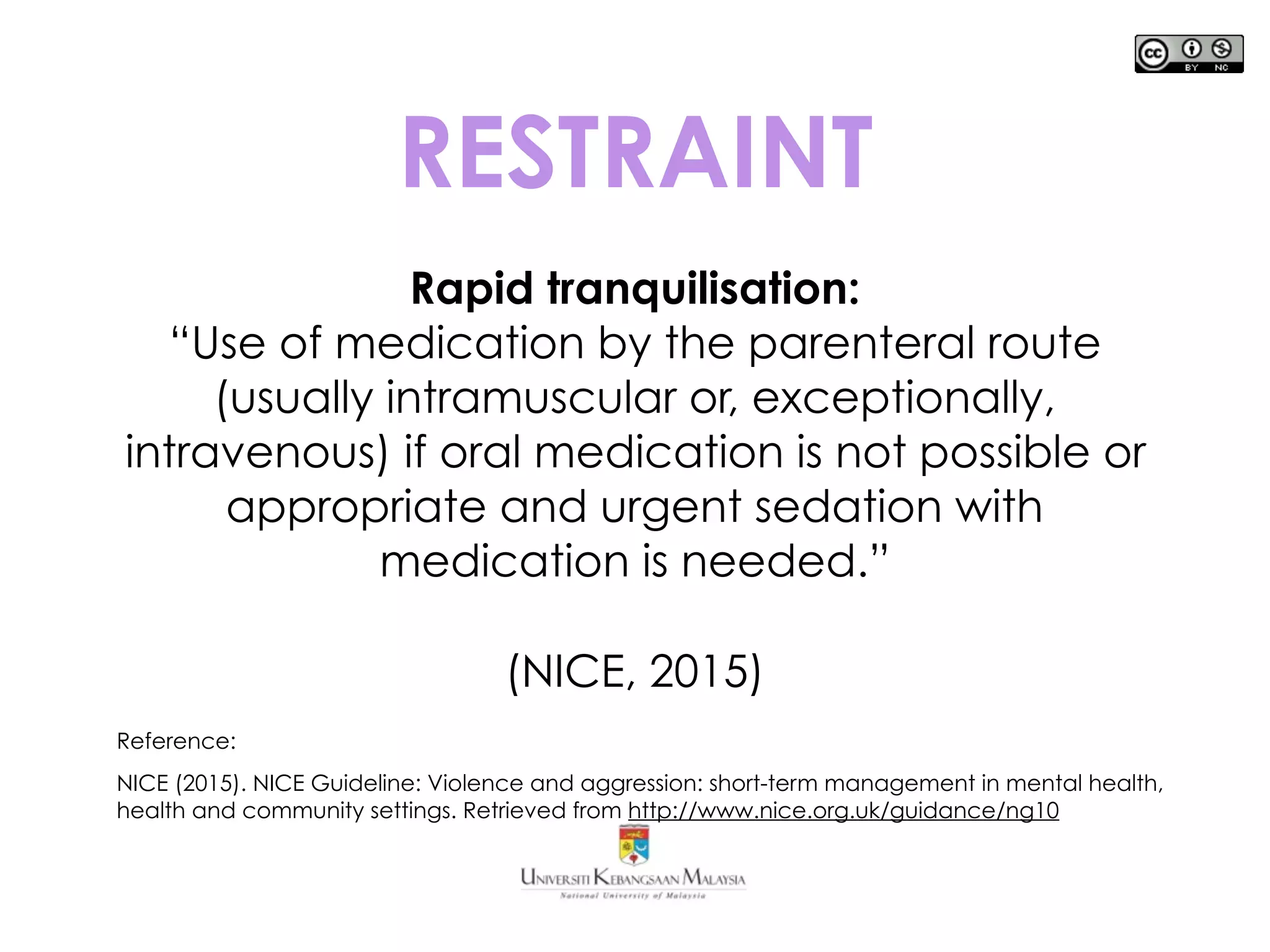
The document discusses seclusion and restraints in emergency psychiatry. It describes the different types of seclusion, restraints, and how to reduce their use. Seclusion involves confining a disturbed patient alone in a locked room to contain behavior, while restraints physically limit a patient's movement. Both should only be used as a last resort for safety and minimizing time in restraints. Staff must closely monitor patients and prioritize preventative de-escalation techniques to reduce the need for seclusion and restraints.




![From: Neurobiology of Aggression and Violence
American Journal of Psychiatry
Figure 4. Pretreatment Abnormalities in the Pathophysiology of Aggression
a Figure adapted/modified with permission from S.J. DeArmond et al., “Structure of the Human Brain: A Photographic Atlas, Third
Edition” [Oxford University Press, New York, 1989]. Copyright © Oxford University Press. A modified version of this figure
appeared in Davidson et al., Science 2000; 289:591.
Copyright © American Psychiatric Association.
All rights reserved.
Date of download:
09/19/2015](https://image.slidesharecdn.com/restraints-150930130504-lva1-app6891/75/Seclusion-and-Restraints-15-2048.jpg)
![From: Neurobiology of Aggression and Violence
American Journal of Psychiatry
Figure 5. Posttreatment Abnormalities in the Pathophysiology of Aggression
a Figure adapted/modified with permission from S.J. DeArmond et al., “Structure of the Human Brain: A Photographic Atlas, Third
Edition” [Oxford University Press, New York, 1989]. Copyright © Oxford University Press. A modified version of this figure
appeared in Davidson et al., Science 2000; 289:591.
Copyright © American Psychiatric Association.
All rights reserved.
Date of download:
09/19/2015](https://image.slidesharecdn.com/restraints-150930130504-lva1-app6891/75/Seclusion-and-Restraints-17-2048.jpg)