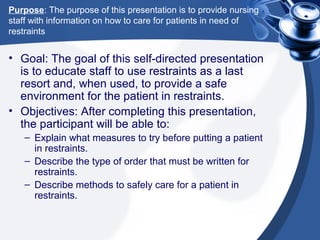
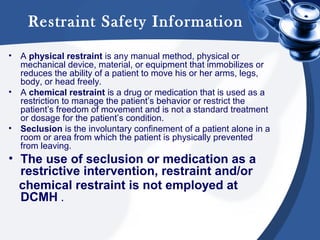
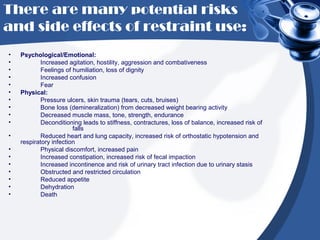
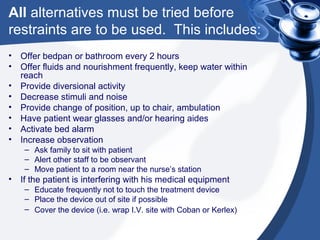
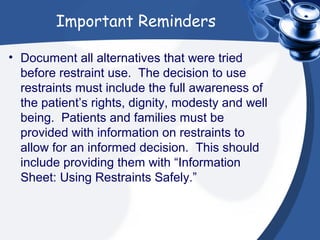
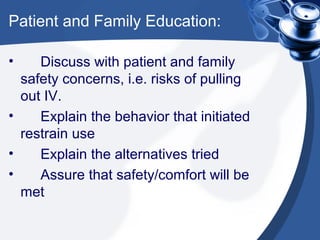
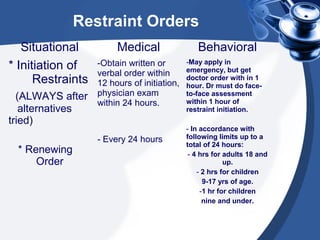
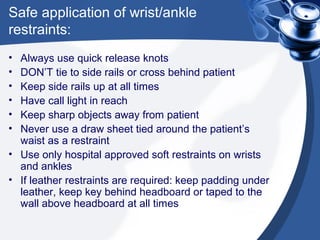
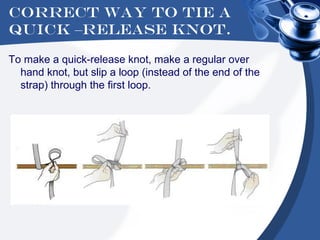
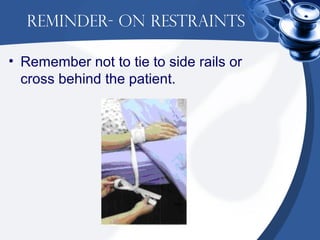
This presentation provides nursing staff education on safely restraining patients when necessary. It aims to teach alternatives to restraints and safe restraint application and monitoring. Key points include obtaining proper physician orders, using restraints as a last resort, monitoring restrained patients every 15 minutes, and documenting care provided. The goal is to educate on restraint safety and providing a safe environment for restrained patients.