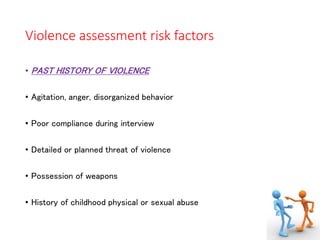
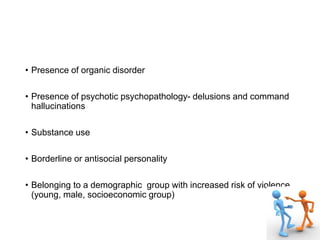
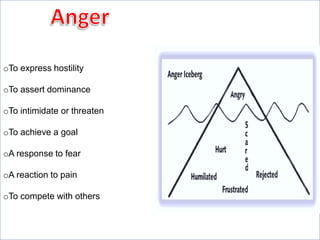
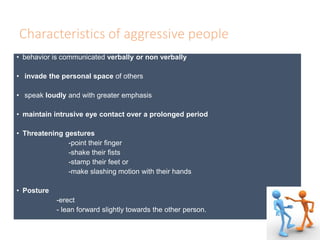
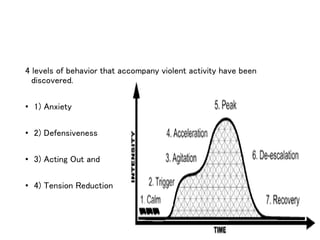
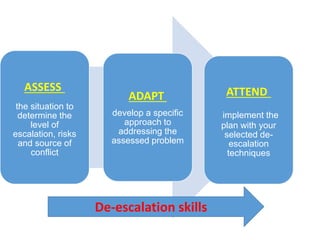
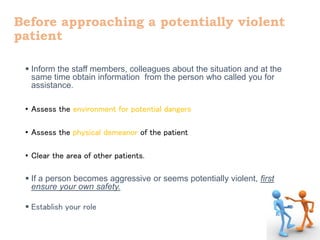
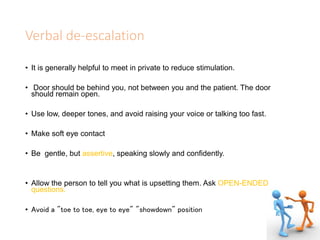
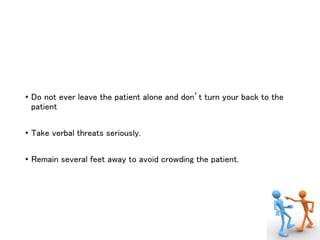
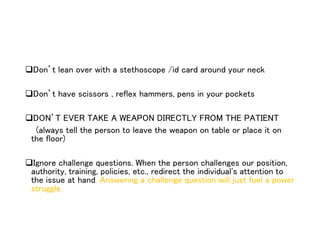
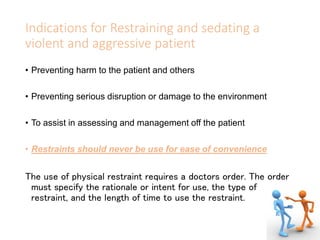
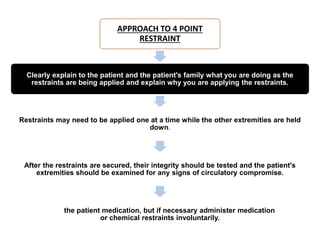
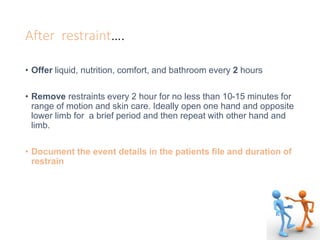
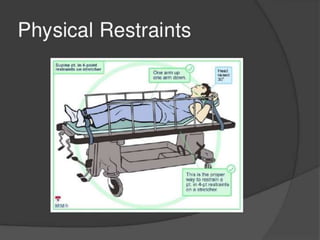
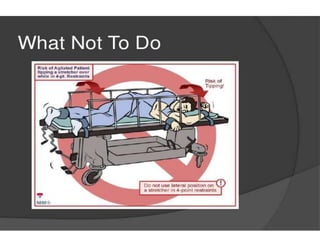
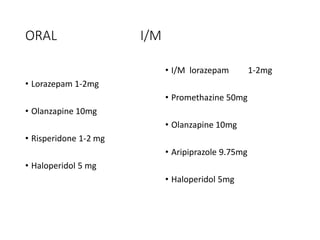
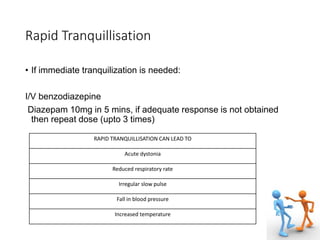
This document discusses the management of aggressive and violent patients. It defines aggression and violence, outlines their causes and risk factors. It describes techniques for assessing risk, de-escalating situations, and restraining or sedating patients if needed. Verbal de-escalation techniques include active listening, empathy, and setting clear boundaries. Physical restraint requires a doctor's order and careful monitoring of the patient's safety and well-being. Chemical restraint options include oral or injectable benzodiazepines and antipsychotics.