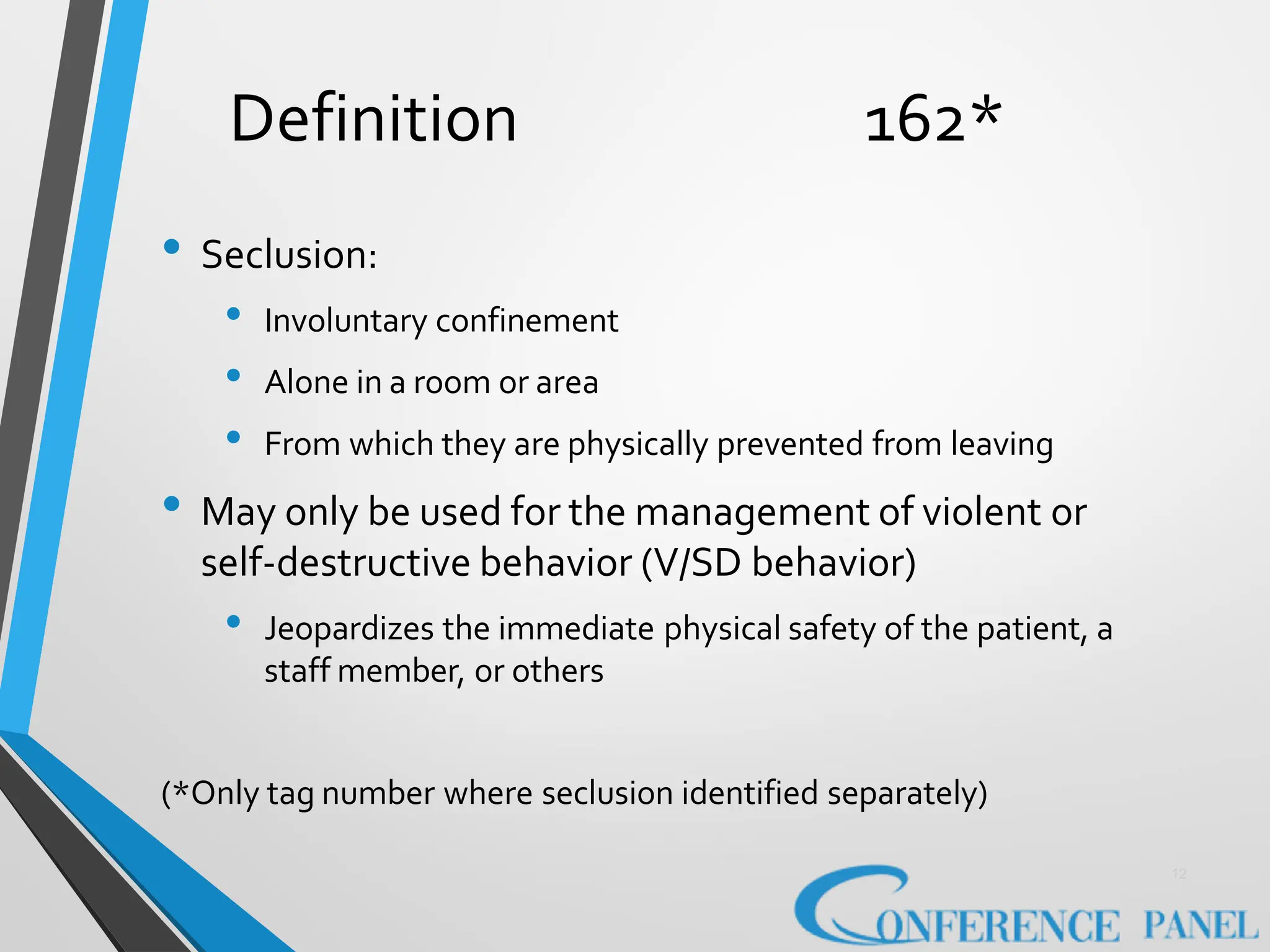
The document discusses the issues surrounding the use of restraint and seclusion in healthcare settings, highlighting the necessity for careful guidelines and documentation to ensure patient safety and minimize adverse effects. It emphasizes that restraints should only be used as a last resort and in a manner that is least restrictive, while also addressing the negative consequences of restraint on both patients and healthcare staff. Additionally, it encourages hospitals to improve staffing levels and implement best practices to reduce the reliance on restraints.