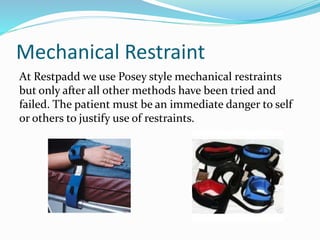
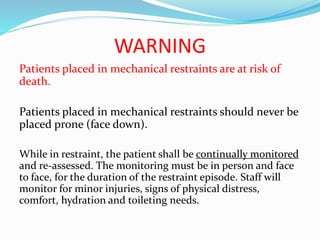
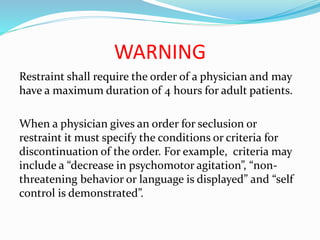
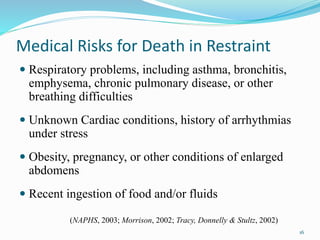
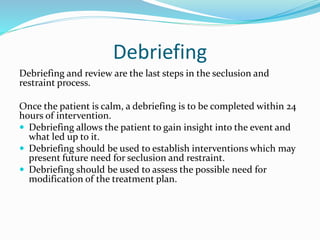
This document provides definitions and guidelines for the use of seclusion and restraint at Restpadd PHF. It defines seclusion as involuntary confinement alone in a room, and restraint as any method that immobilizes or reduces a patient's movement. The facility strives to minimize these practices through proper training and least restrictive methods. These include redirection, reducing stimuli, PRN medications, processing with staff, timeouts, and seclusion or restraint only as a last resort when a patient poses a threat. Medical risks of restraint include respiratory and cardiac issues, and patients must be continually monitored and reassessed if placed in restraints.