Introduction,
Left Heart Catheterization,
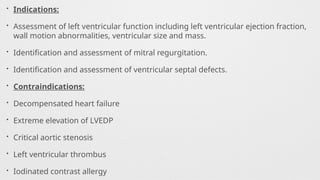
Indications,
Contraindications,
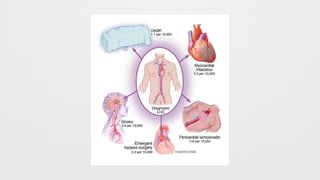
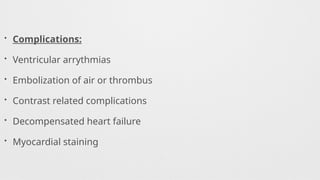
Complications,
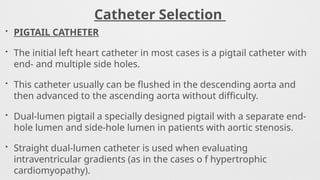
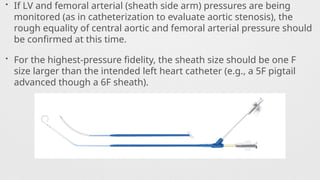
Catheters Used,
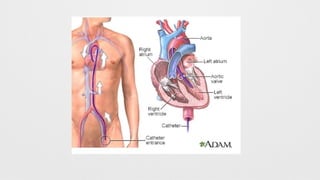
Procedure,
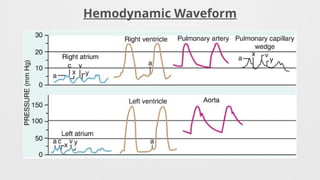
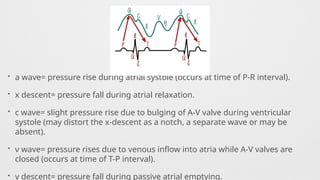
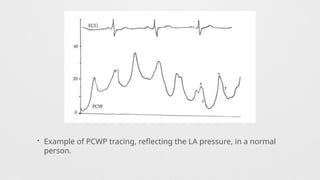
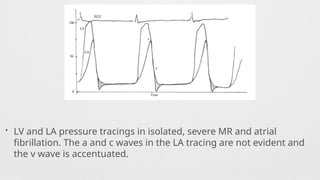
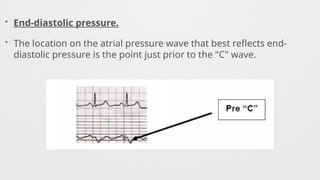
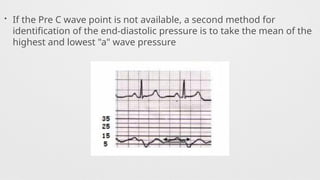
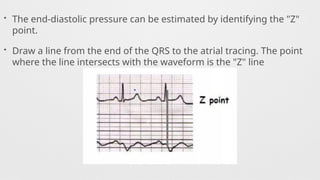
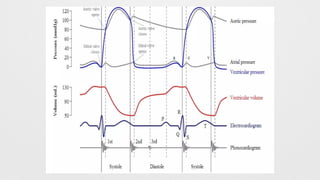
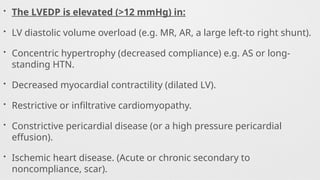
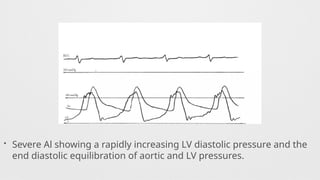
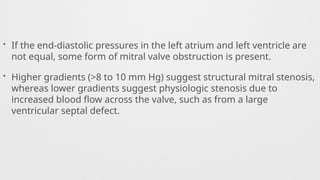
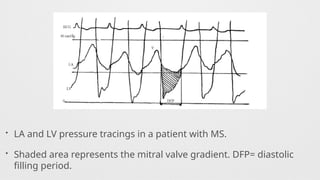
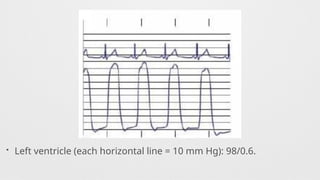
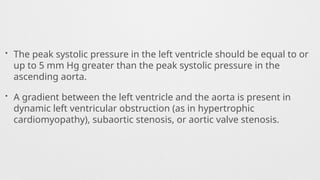
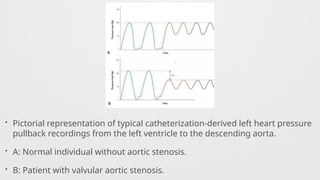
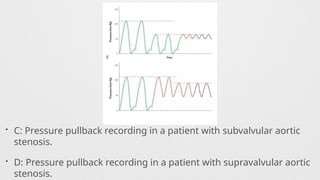
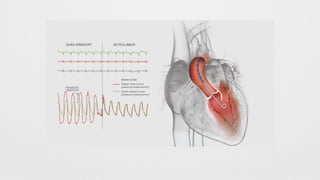
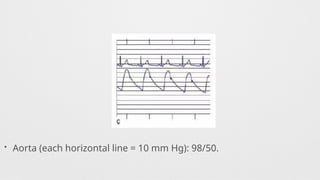
Hemodynamics,
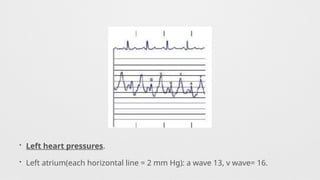
Hemodynamics data,
Shunt Calculation,
Oxymetry,
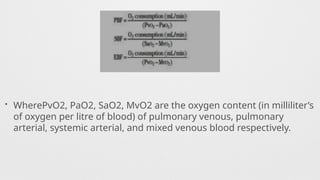
Shunt Quantification,
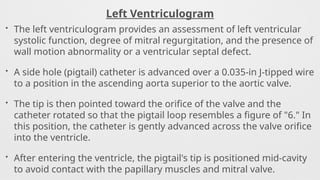
Left Ventriculogram,
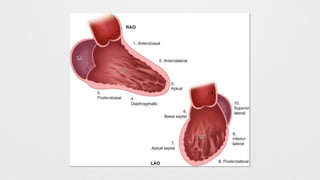
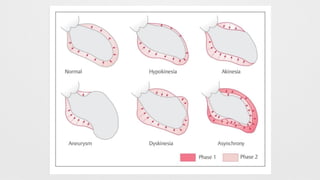
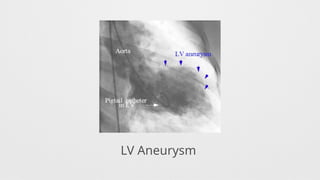
LV Wall motion abnormalities,
Angiographic Aortic Regurgitation,
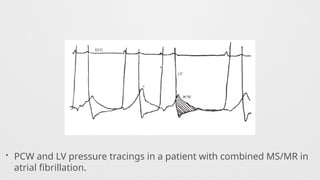
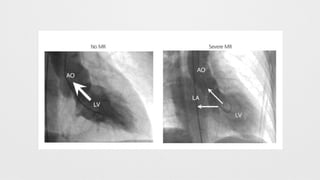
Angiographic Mitral Regurgitation