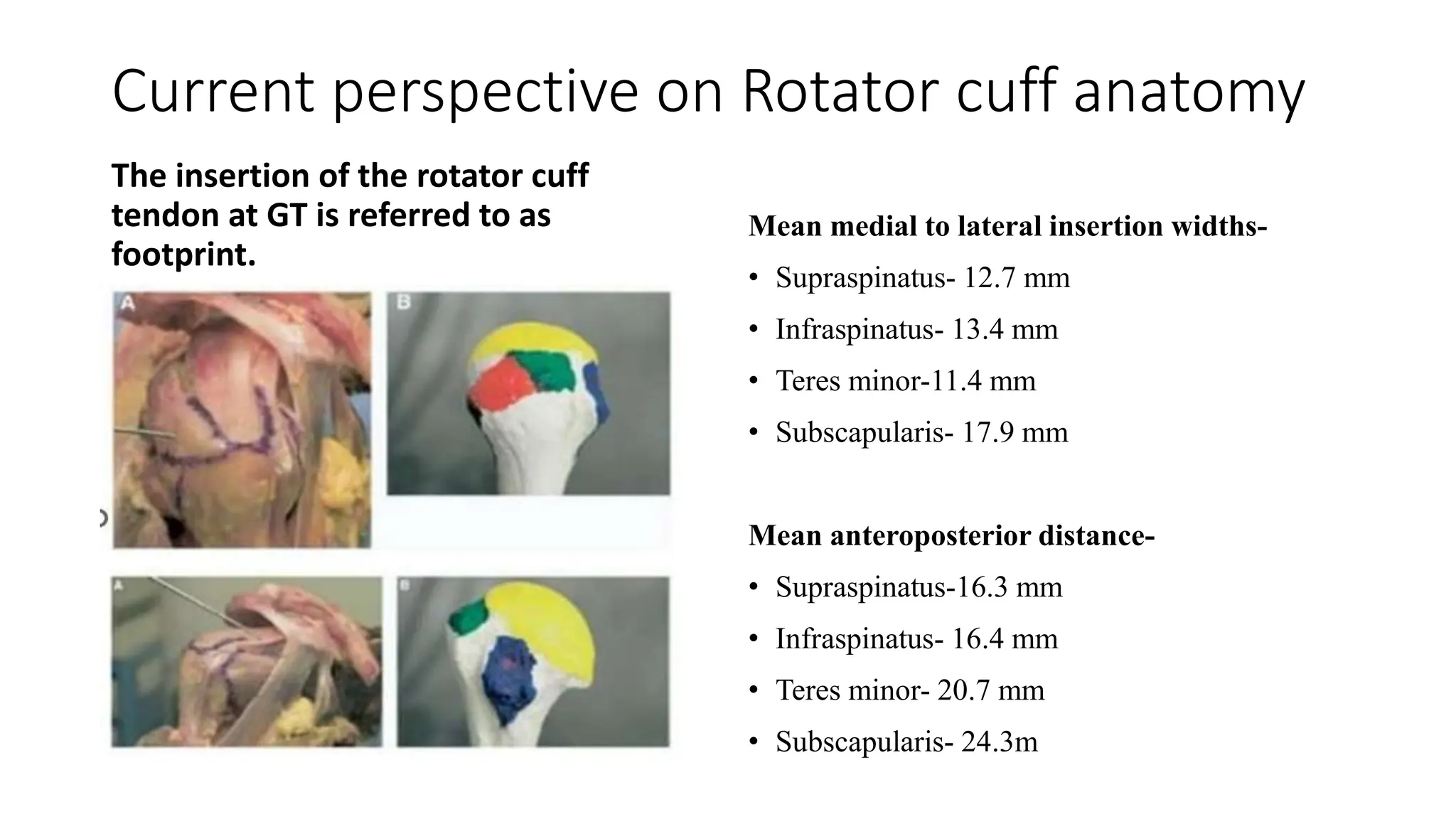
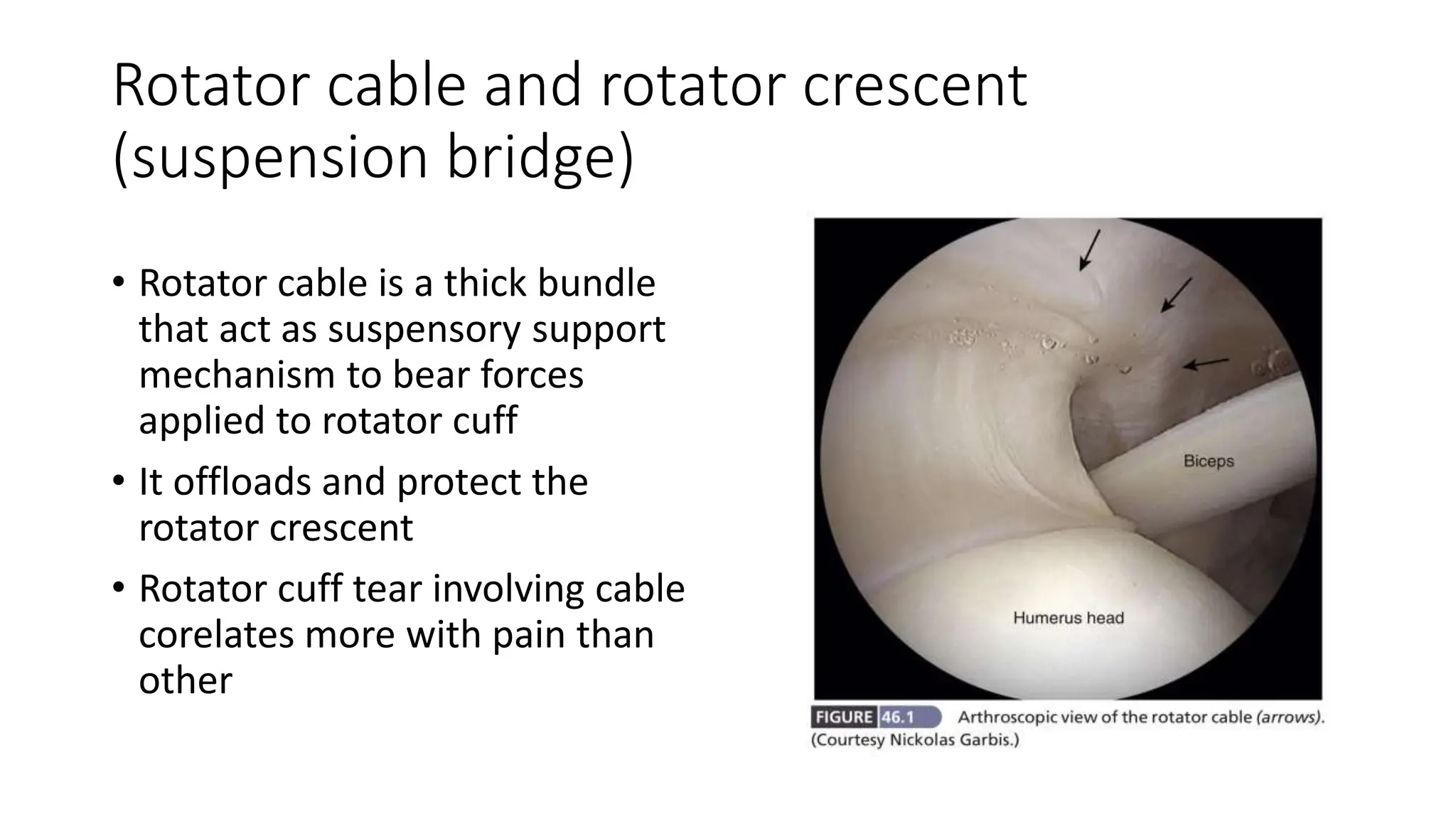
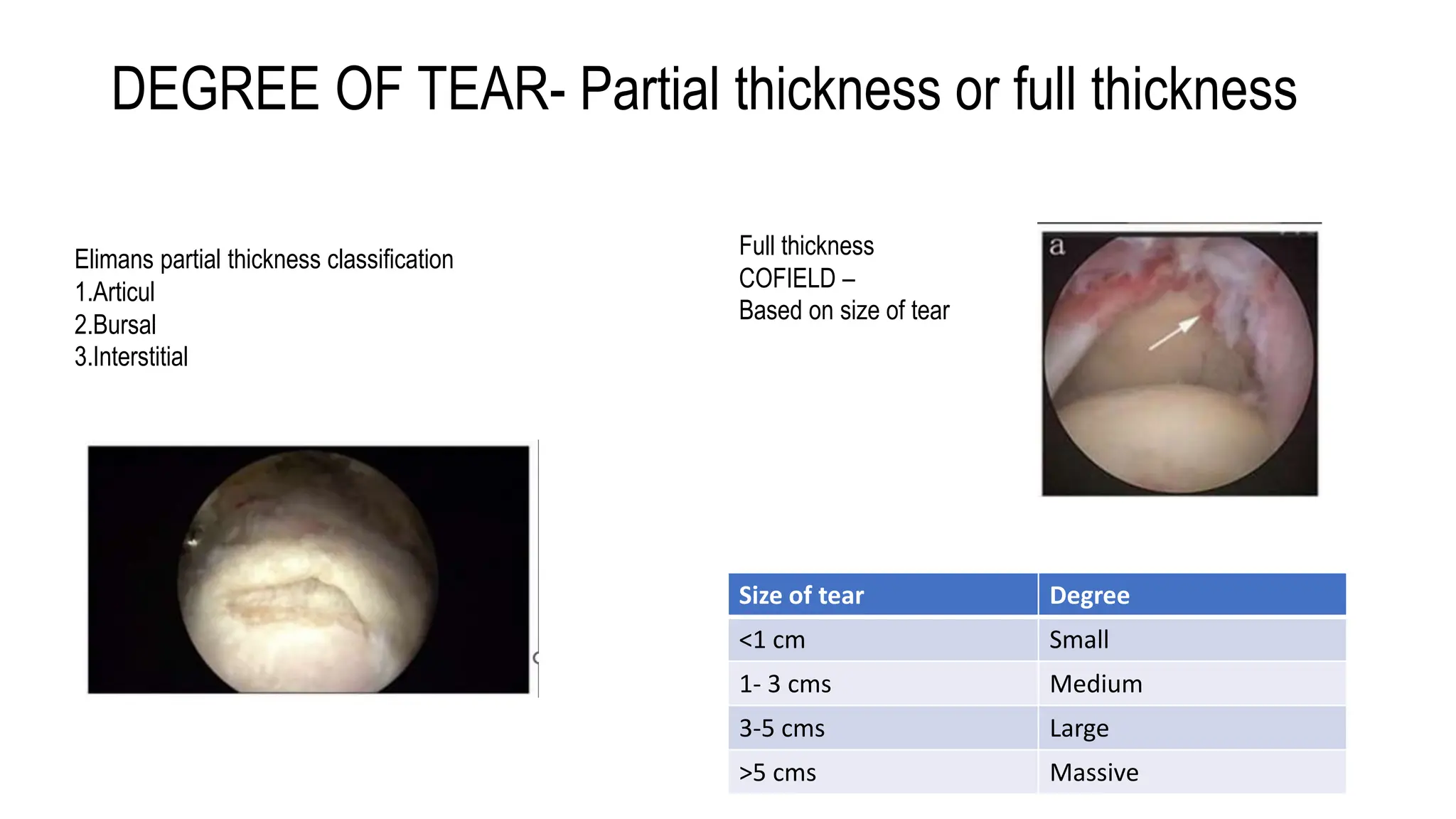
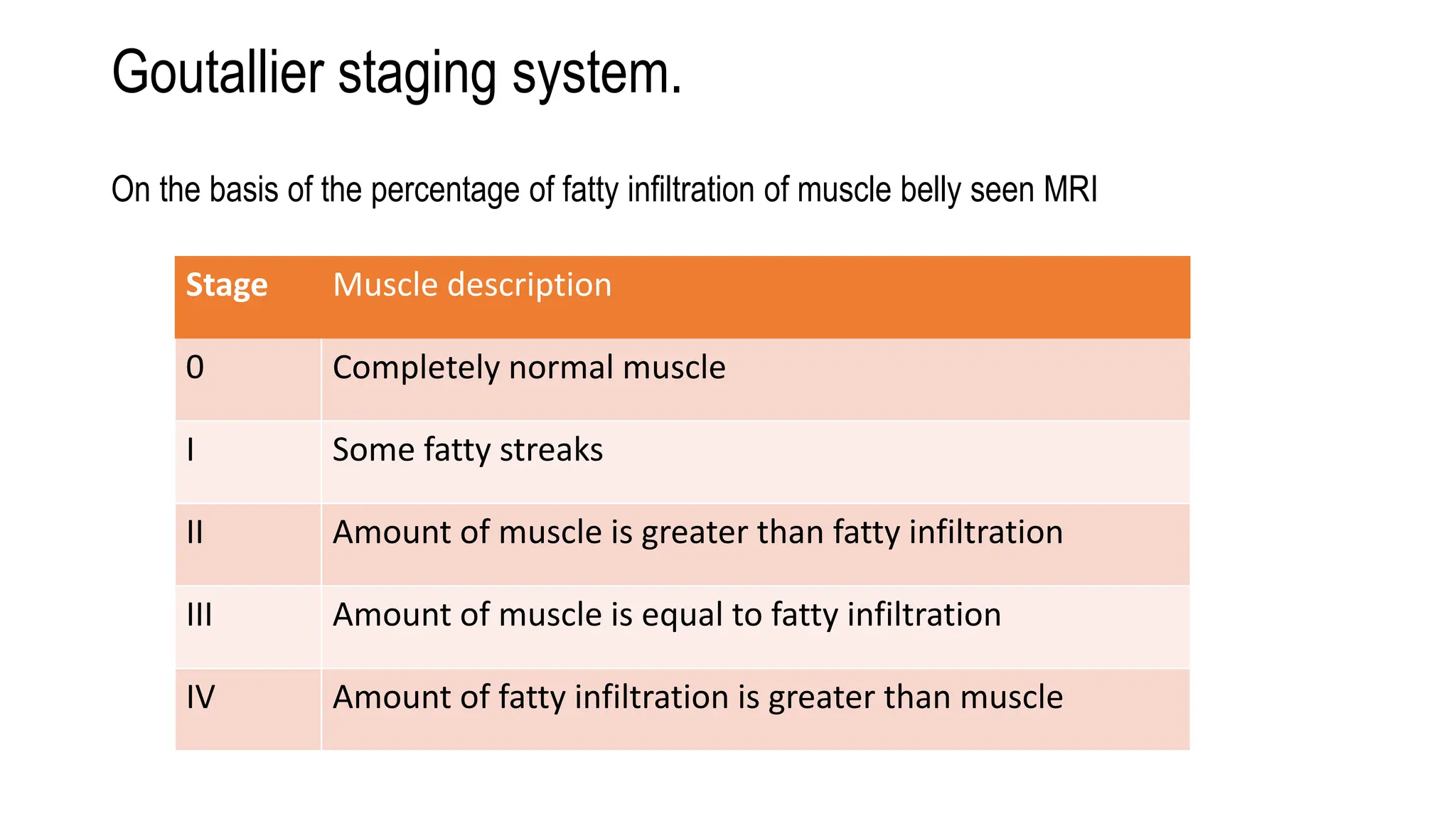
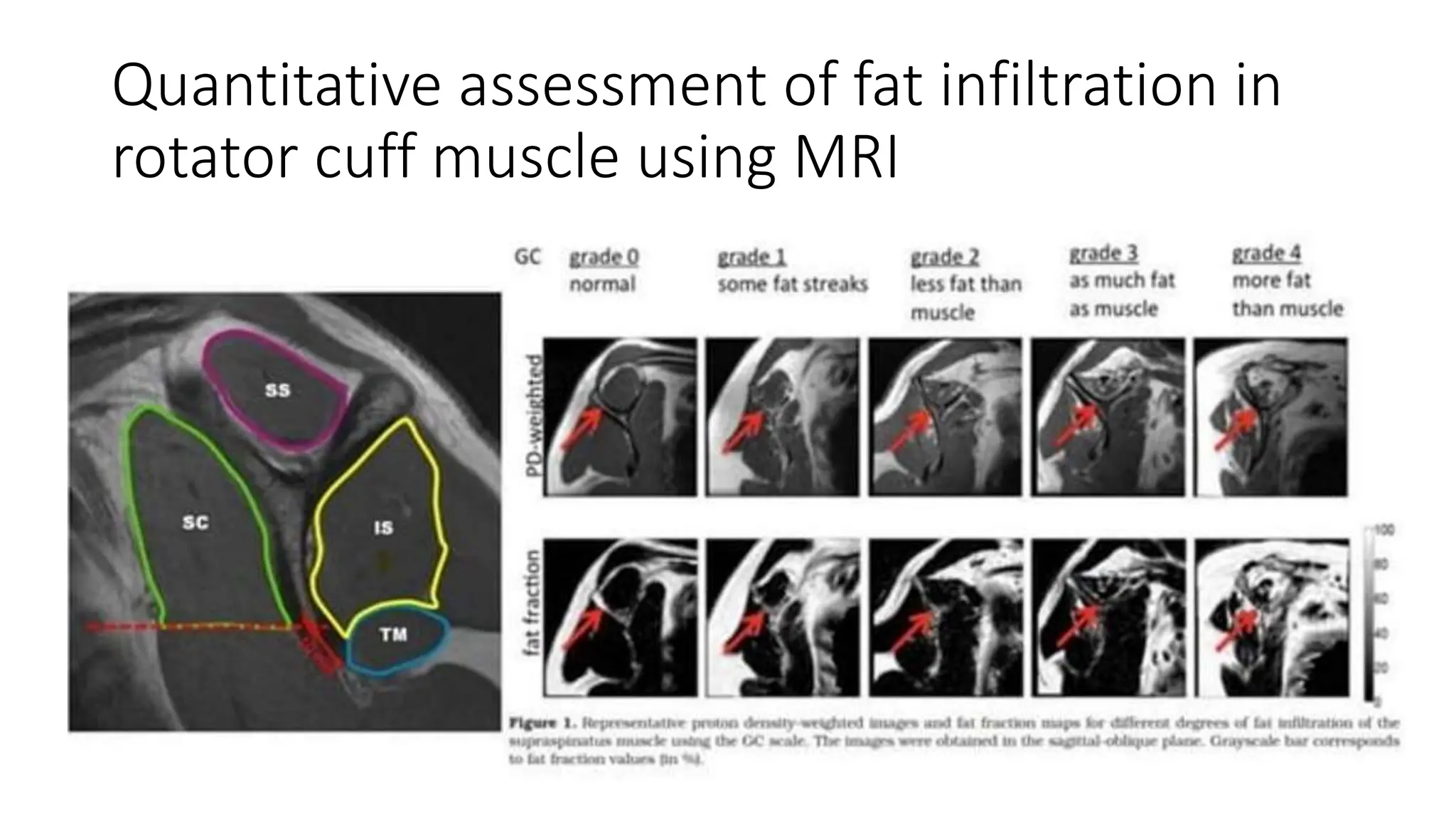
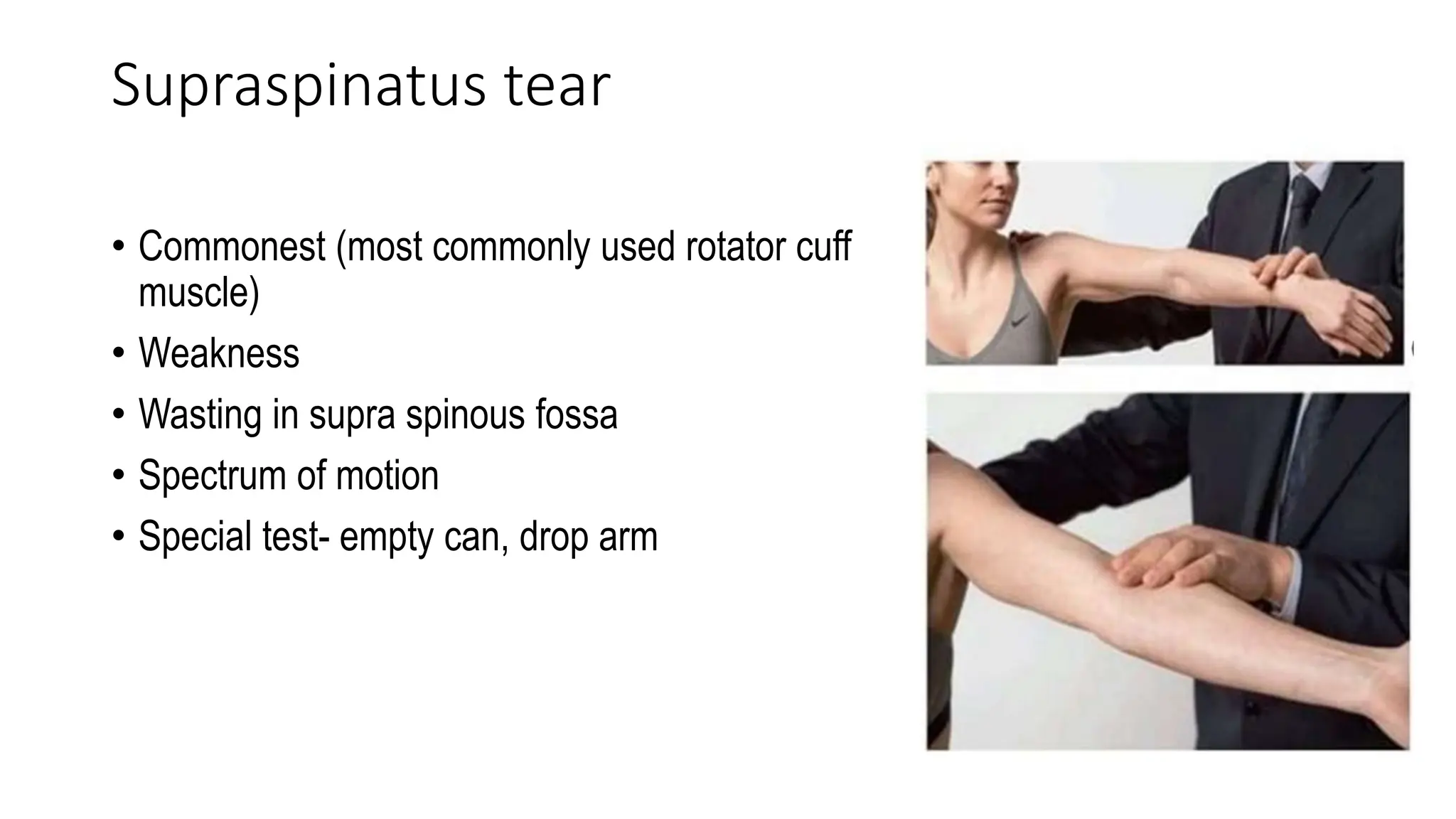
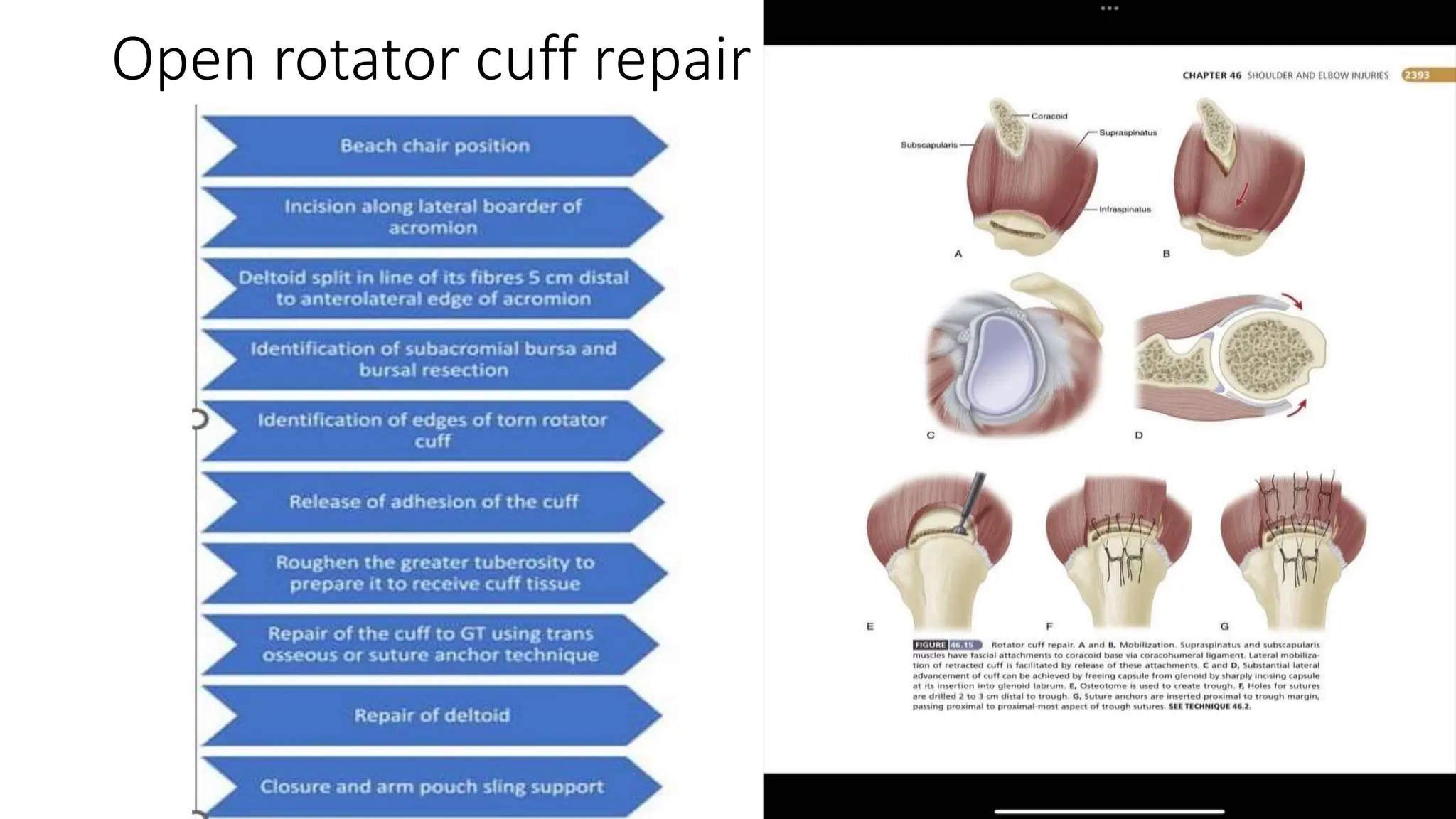
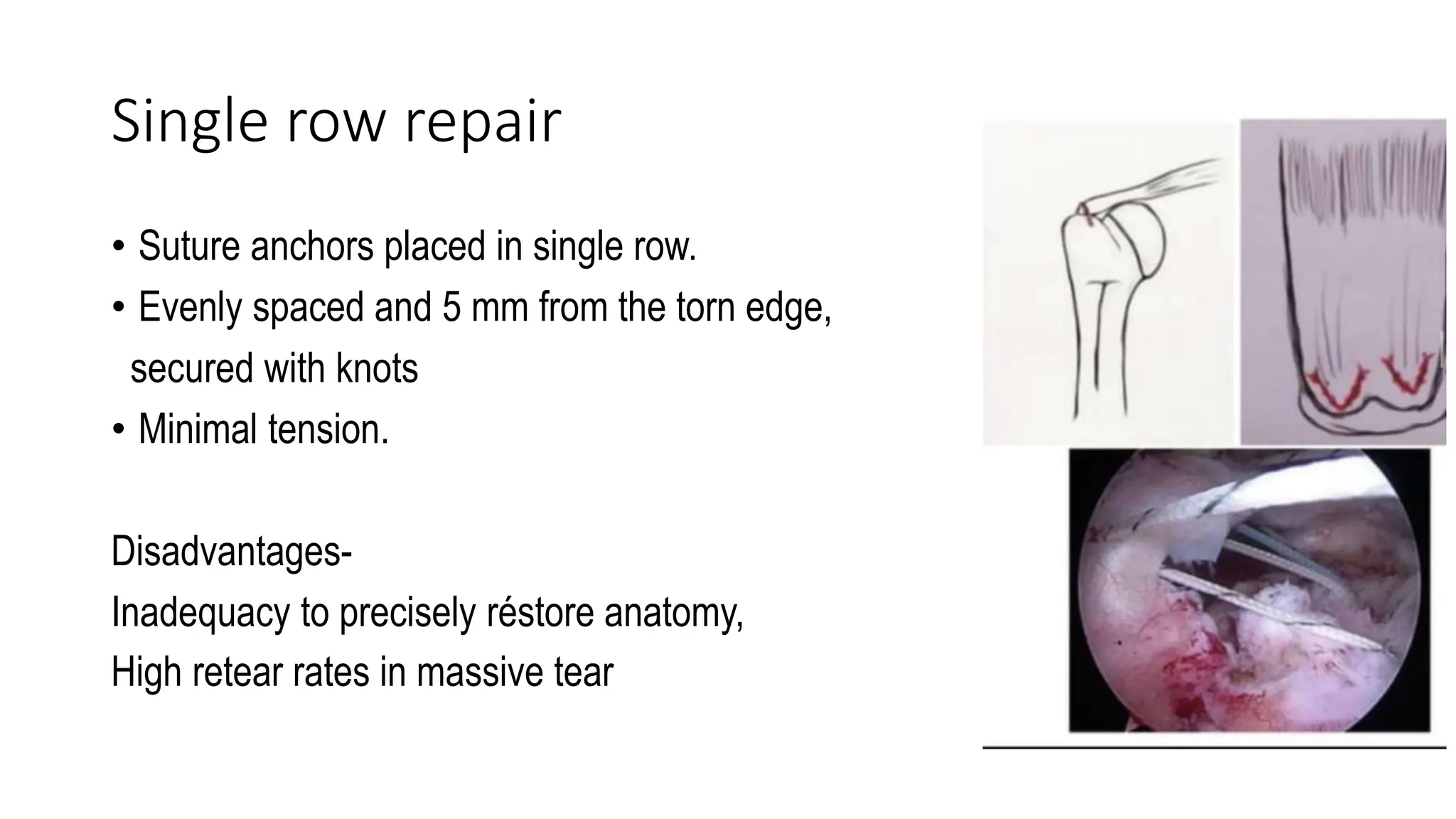
The document discusses rotator cuff injuries, including the anatomy of the rotator cuff, classification of tears, symptoms, physical examinations, investigations like X-rays and MRI, and treatment options like conservative management, open repair, arthroscopic repair, and rehabilitation protocols. It also covers irreparable rotator cuff tears and treatment options for those, which can include conservative care, decompression, tendon transfers, graft interposition, balloon spacers, capsular reconstruction, or reverse shoulder arthroplasty.