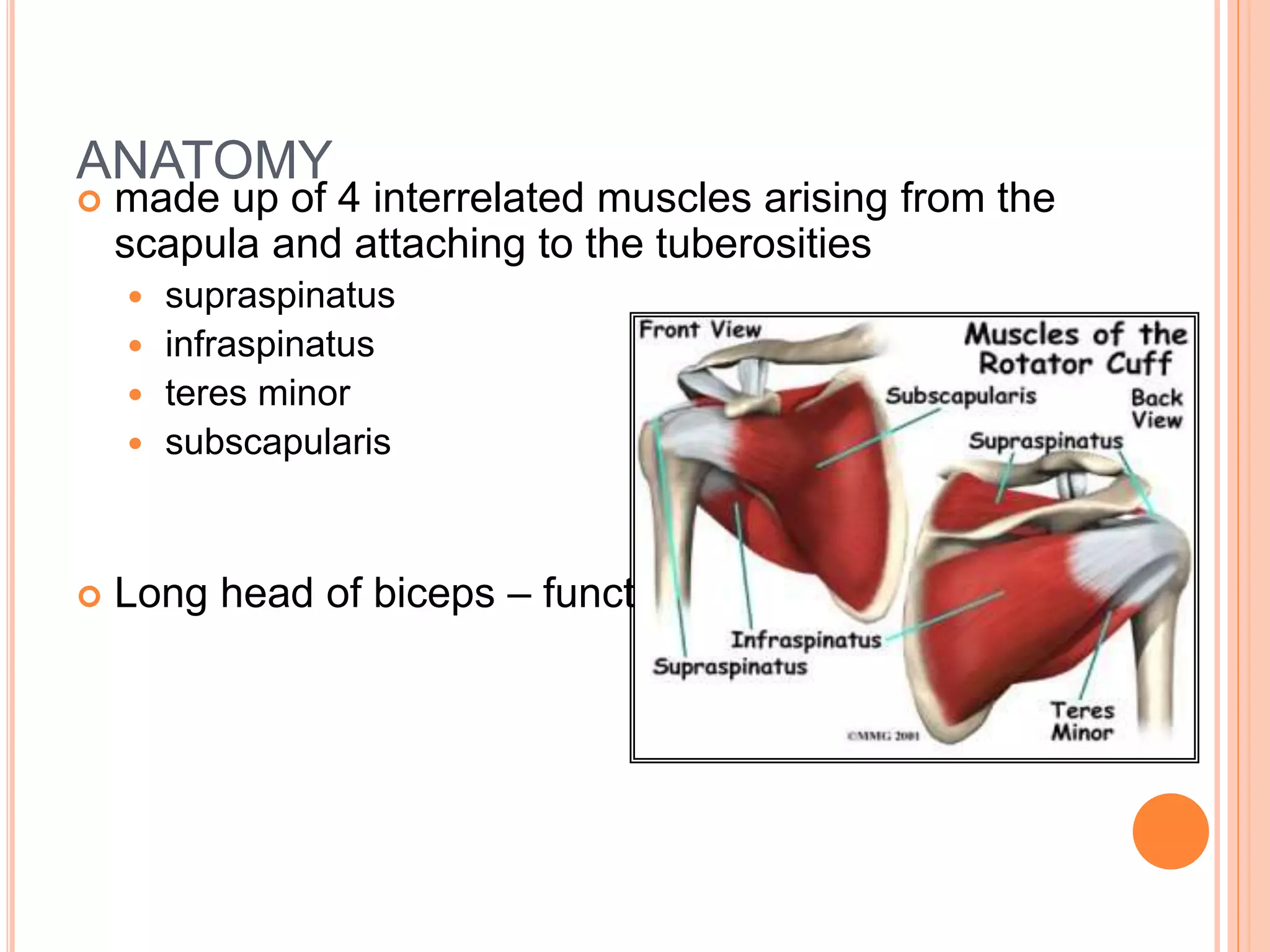
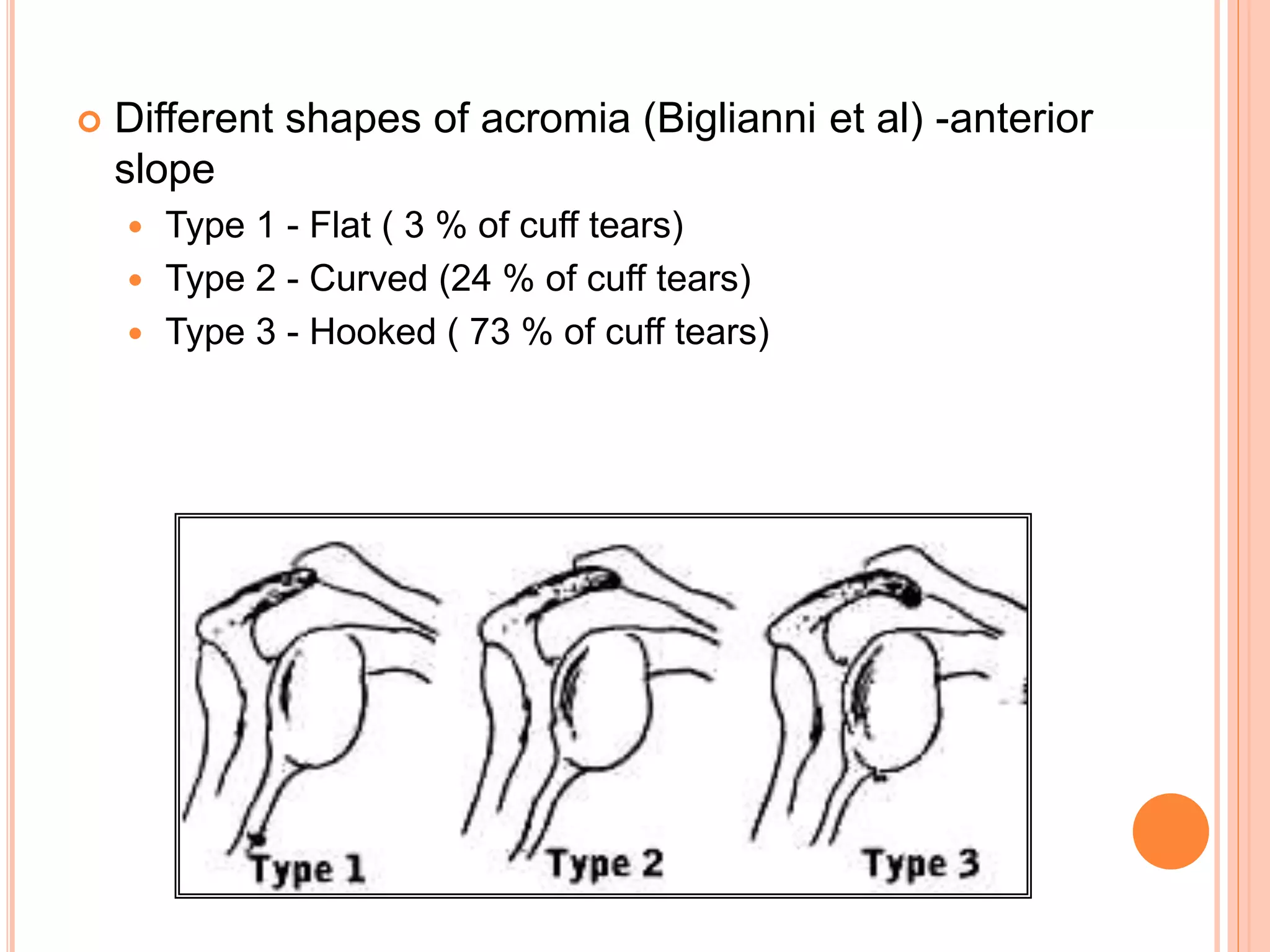
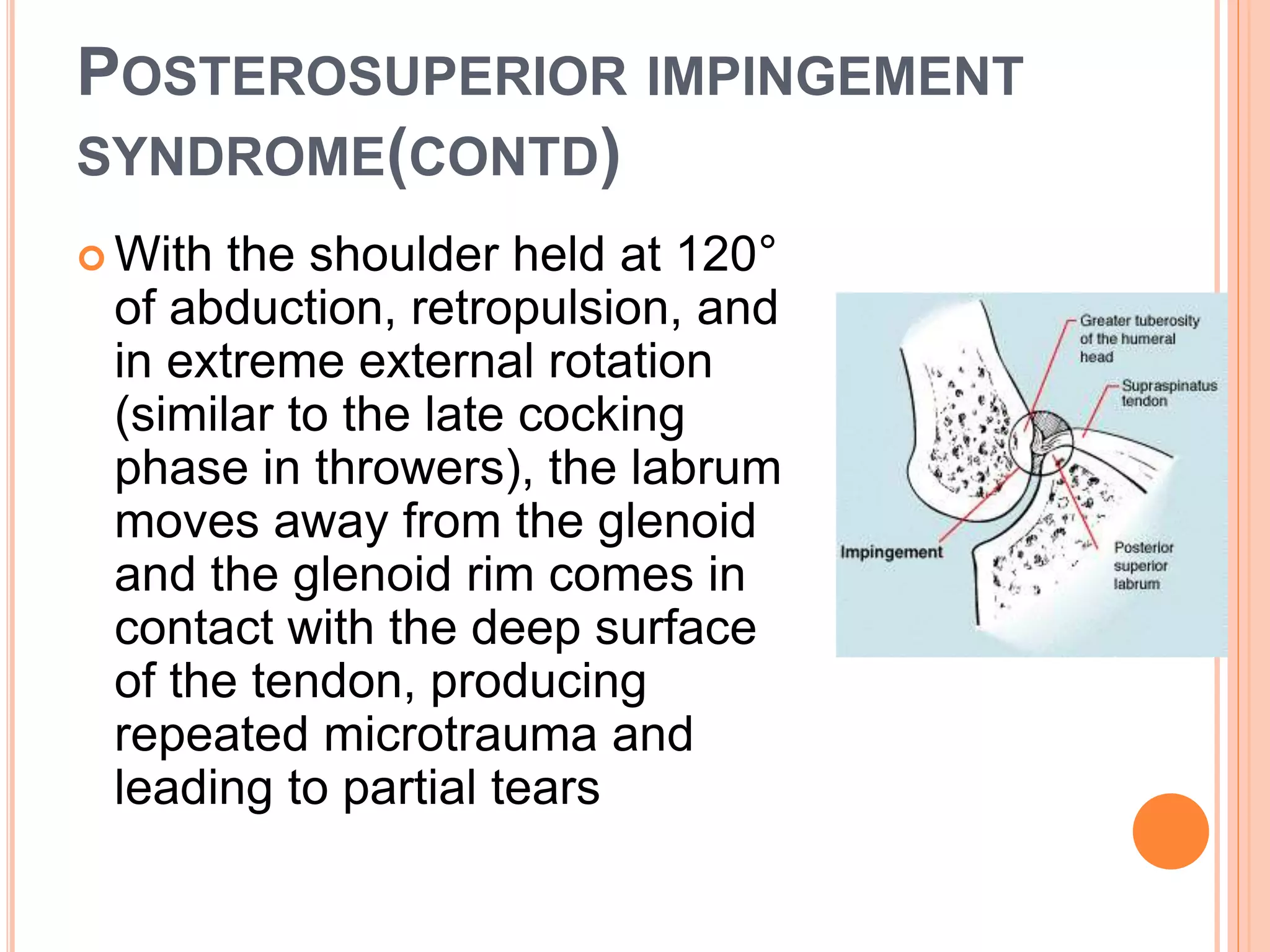
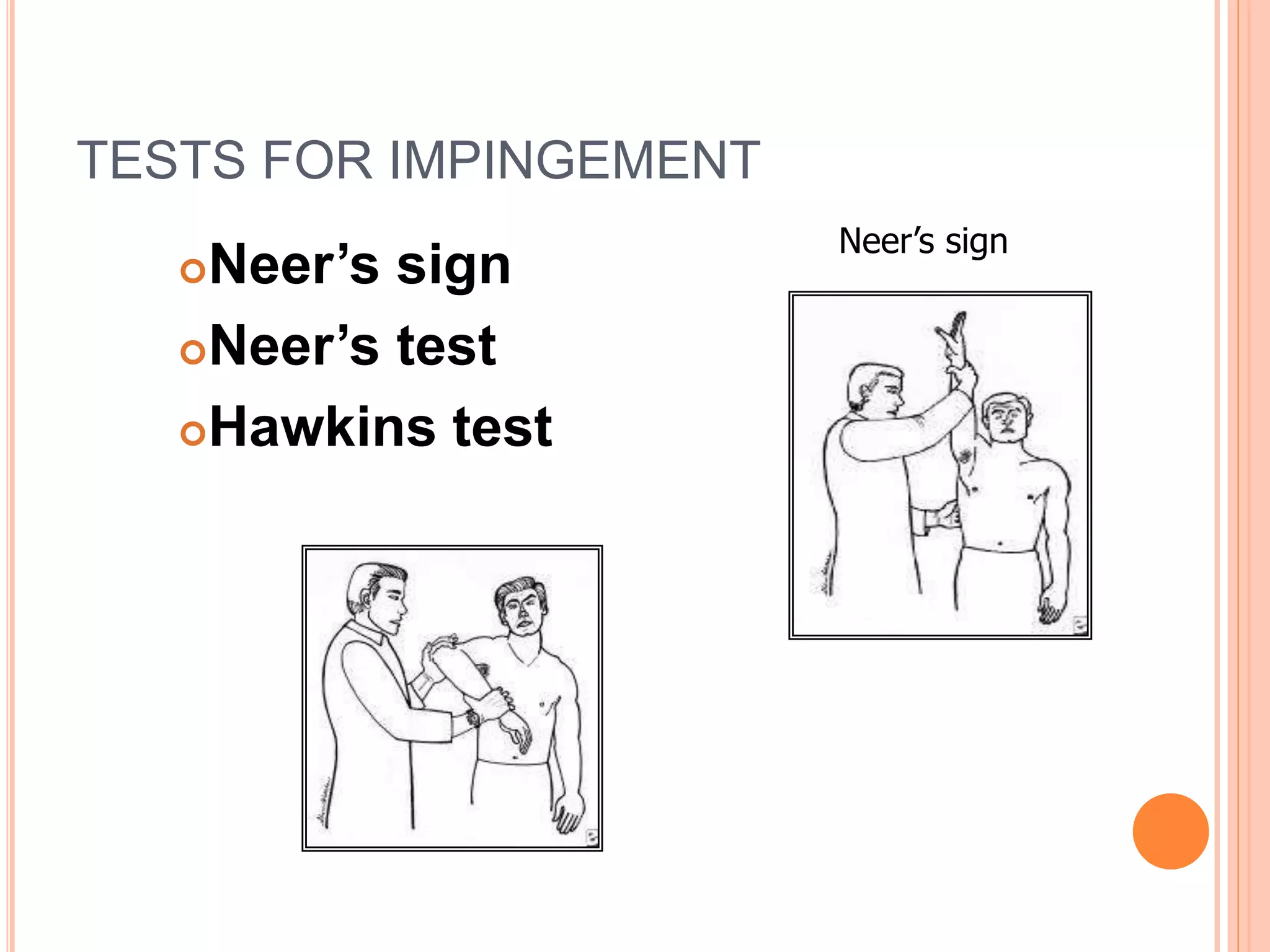
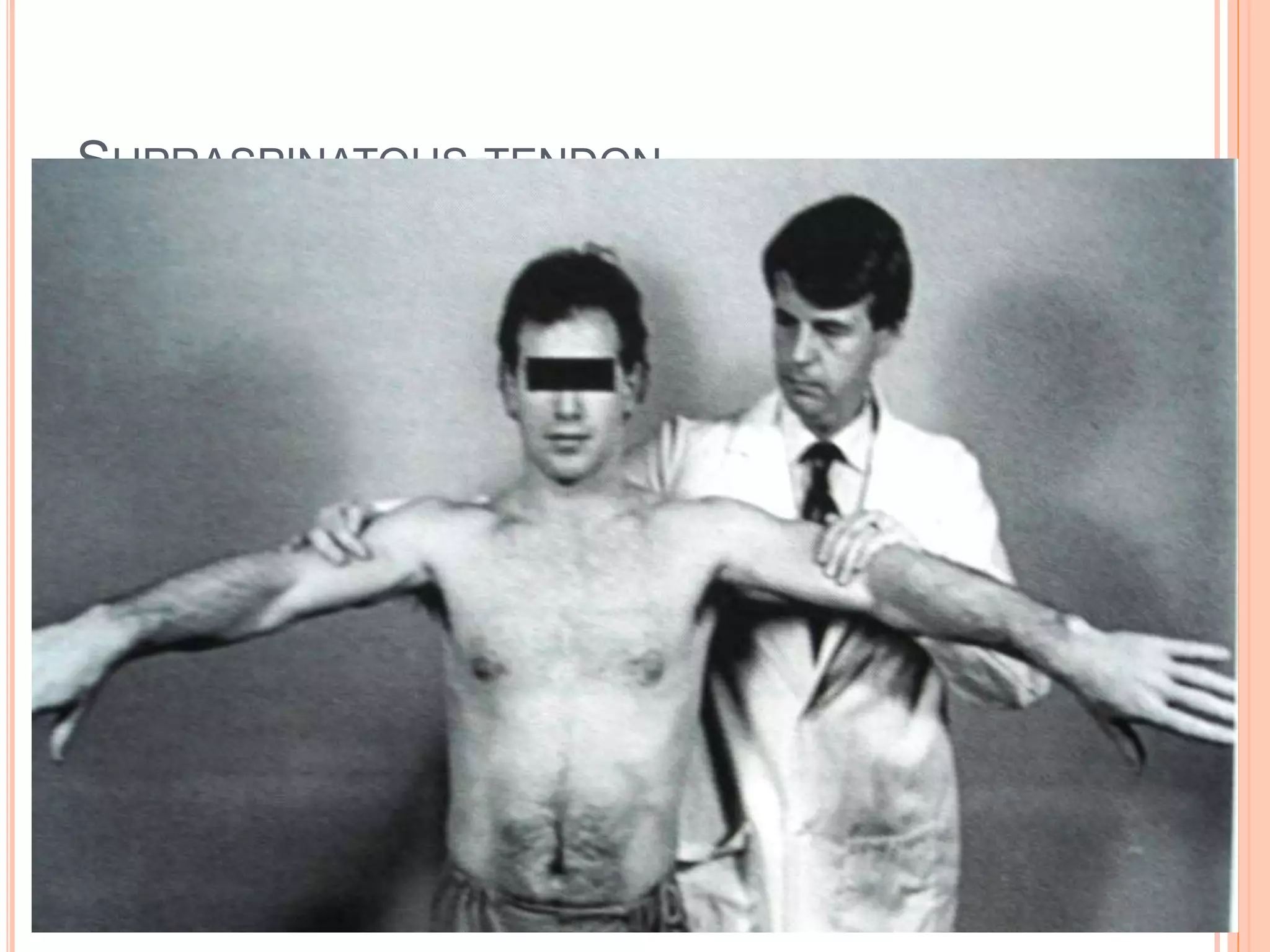
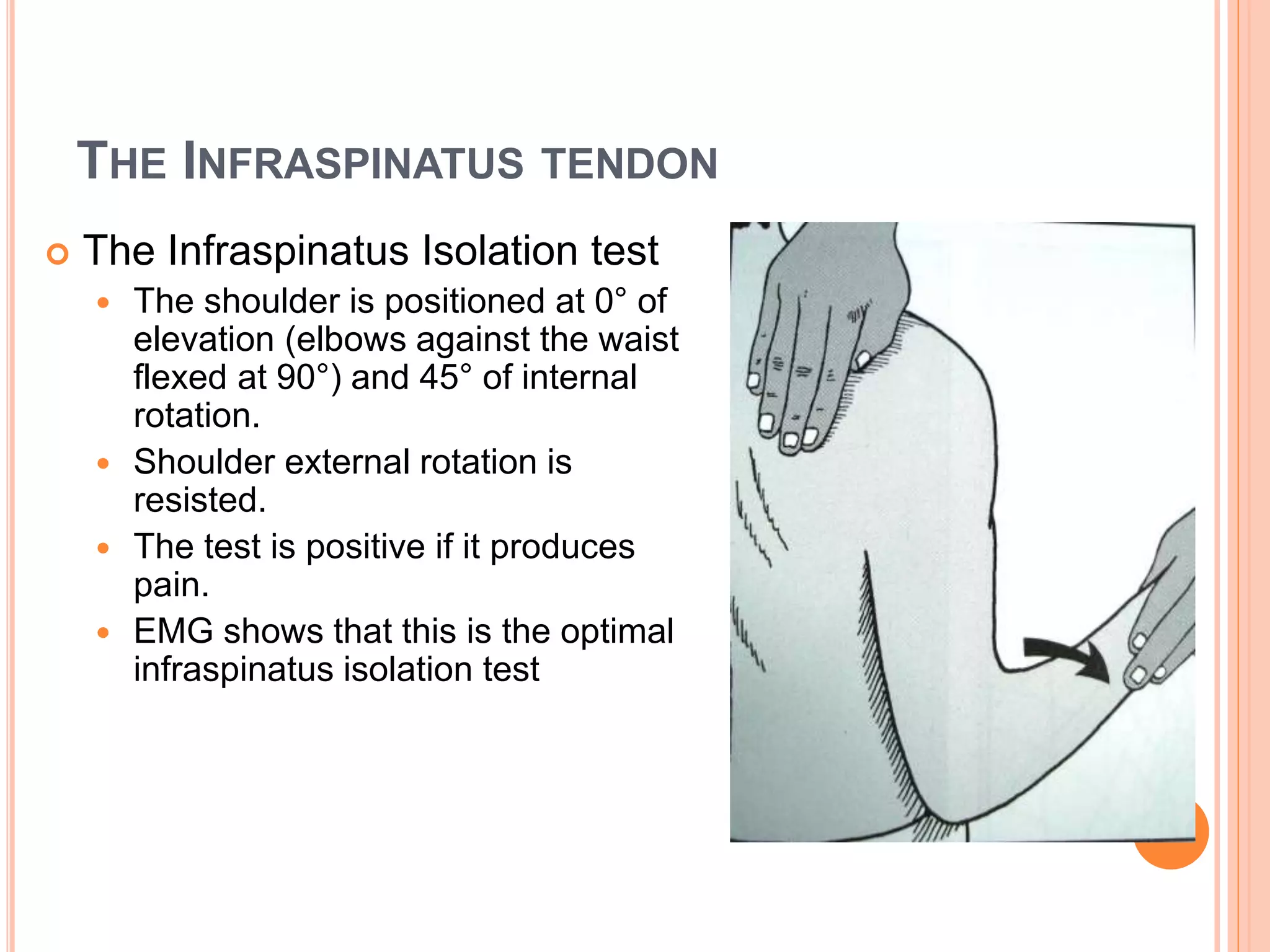
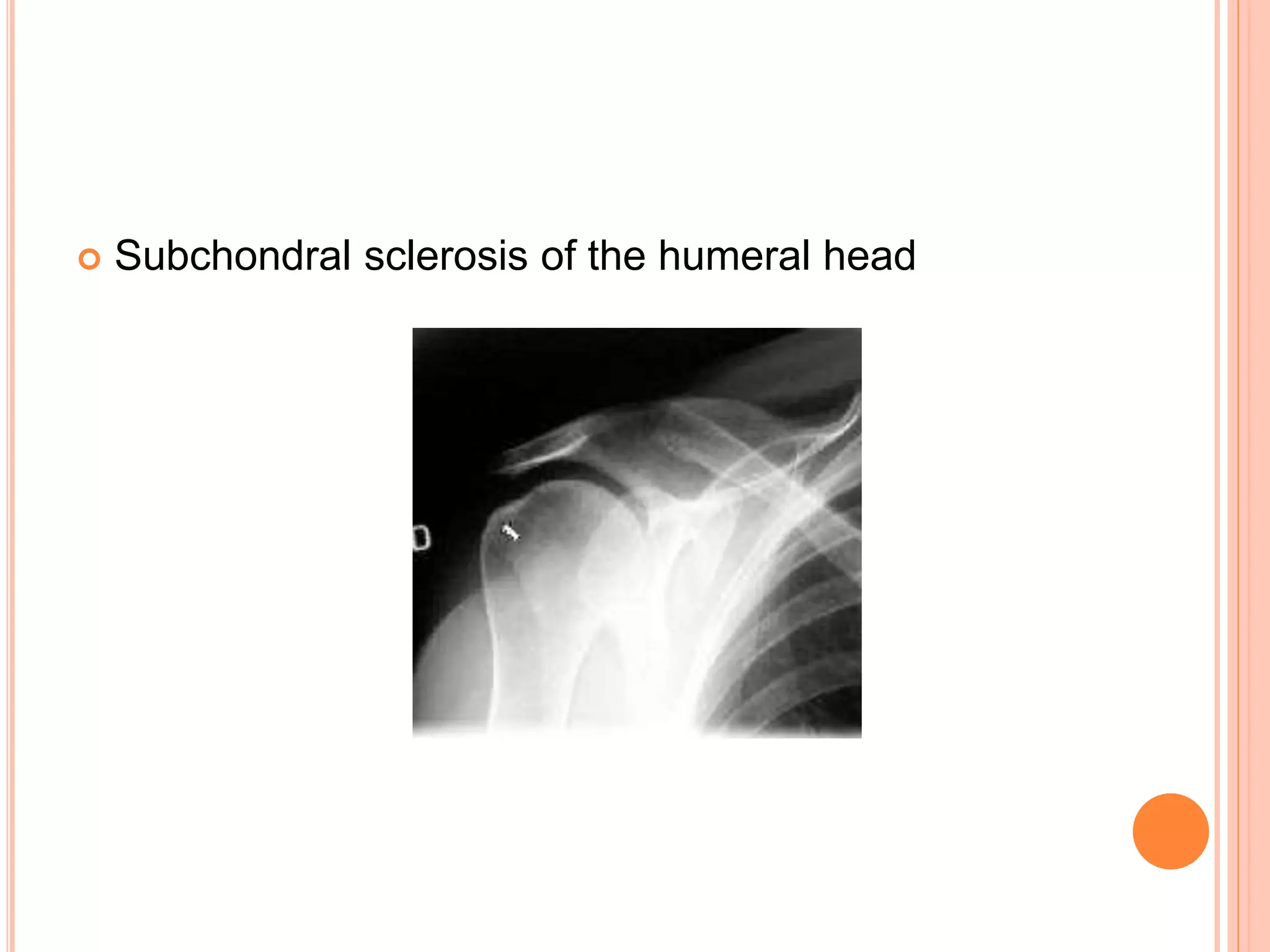
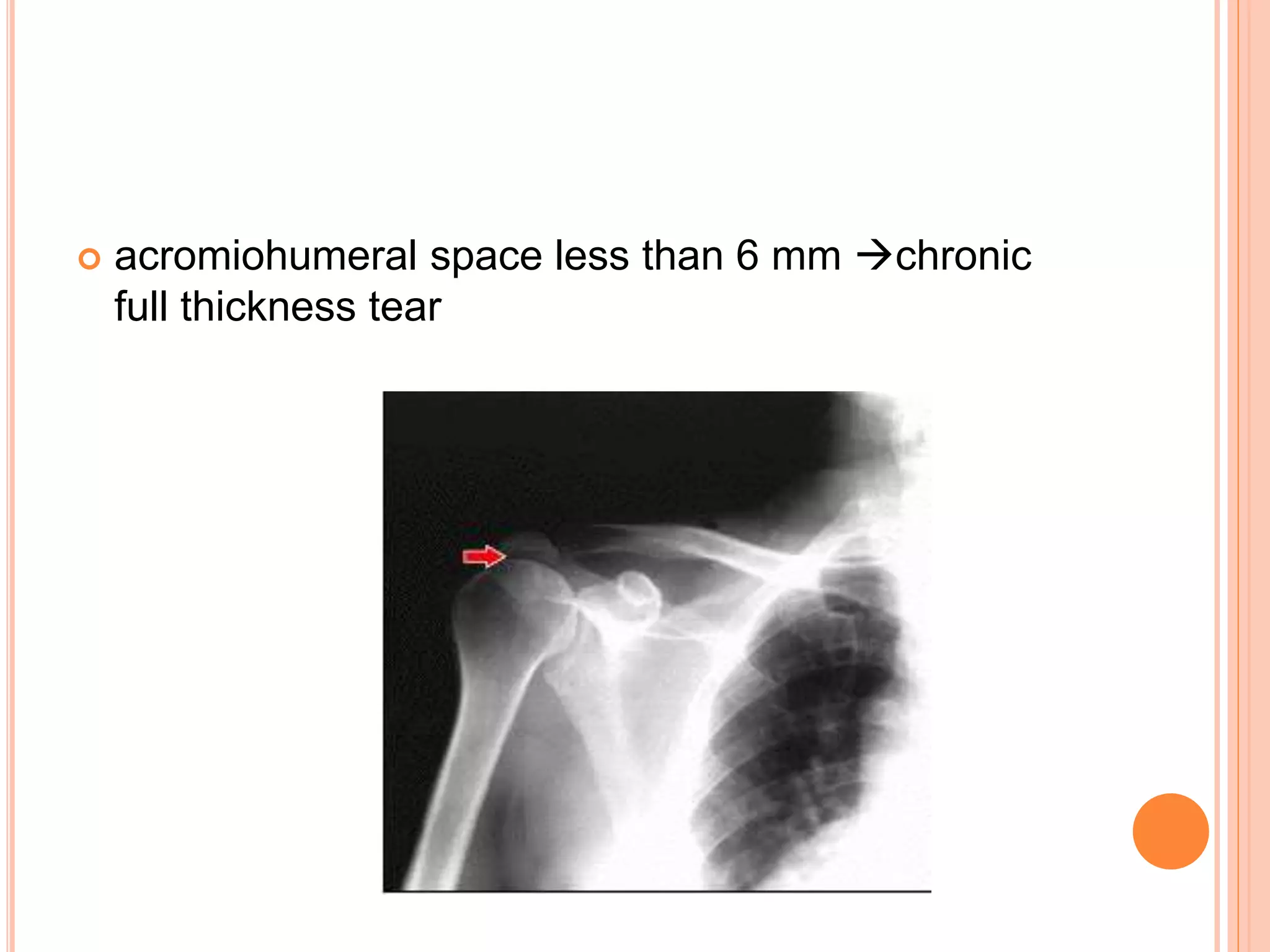
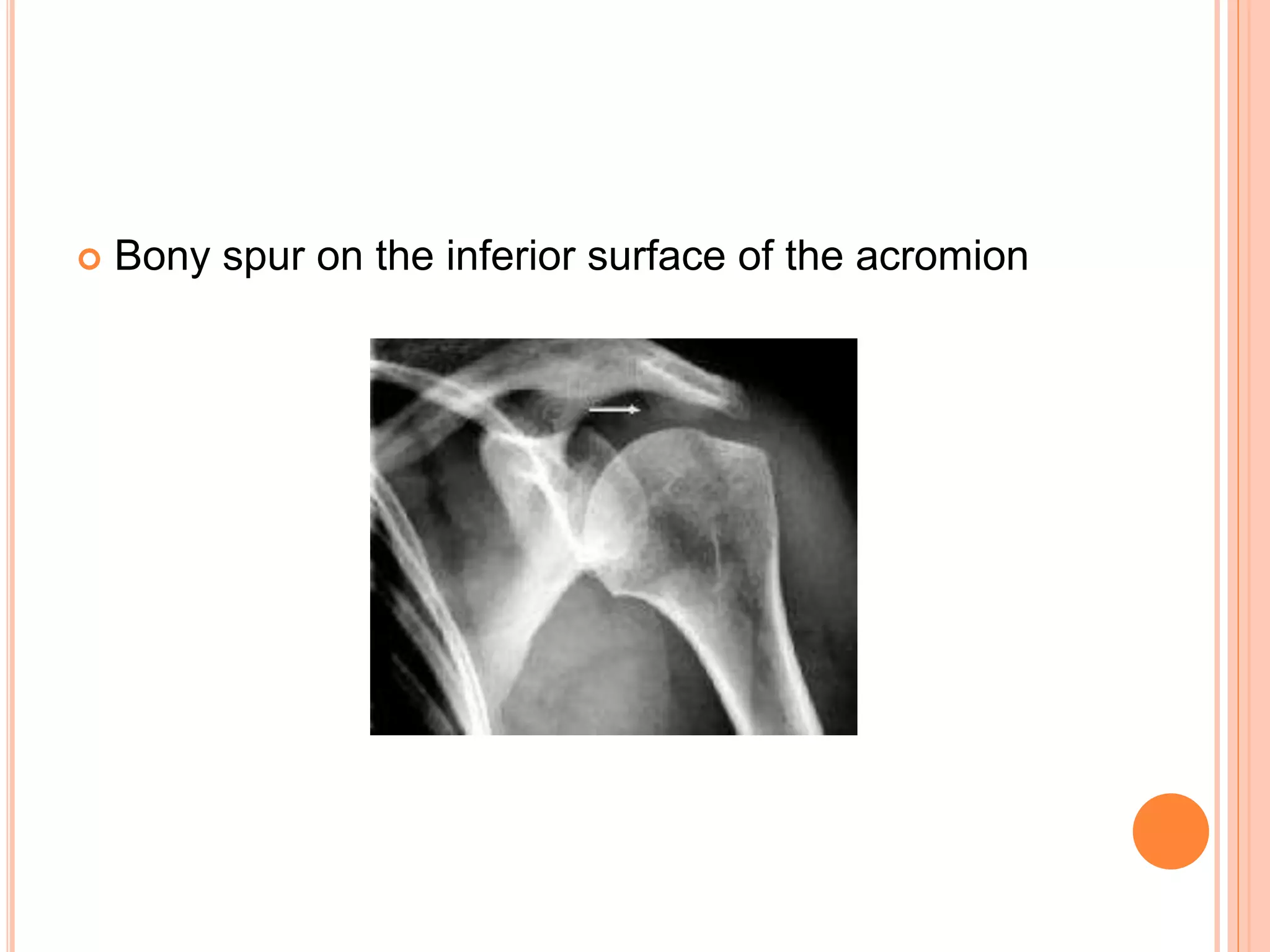
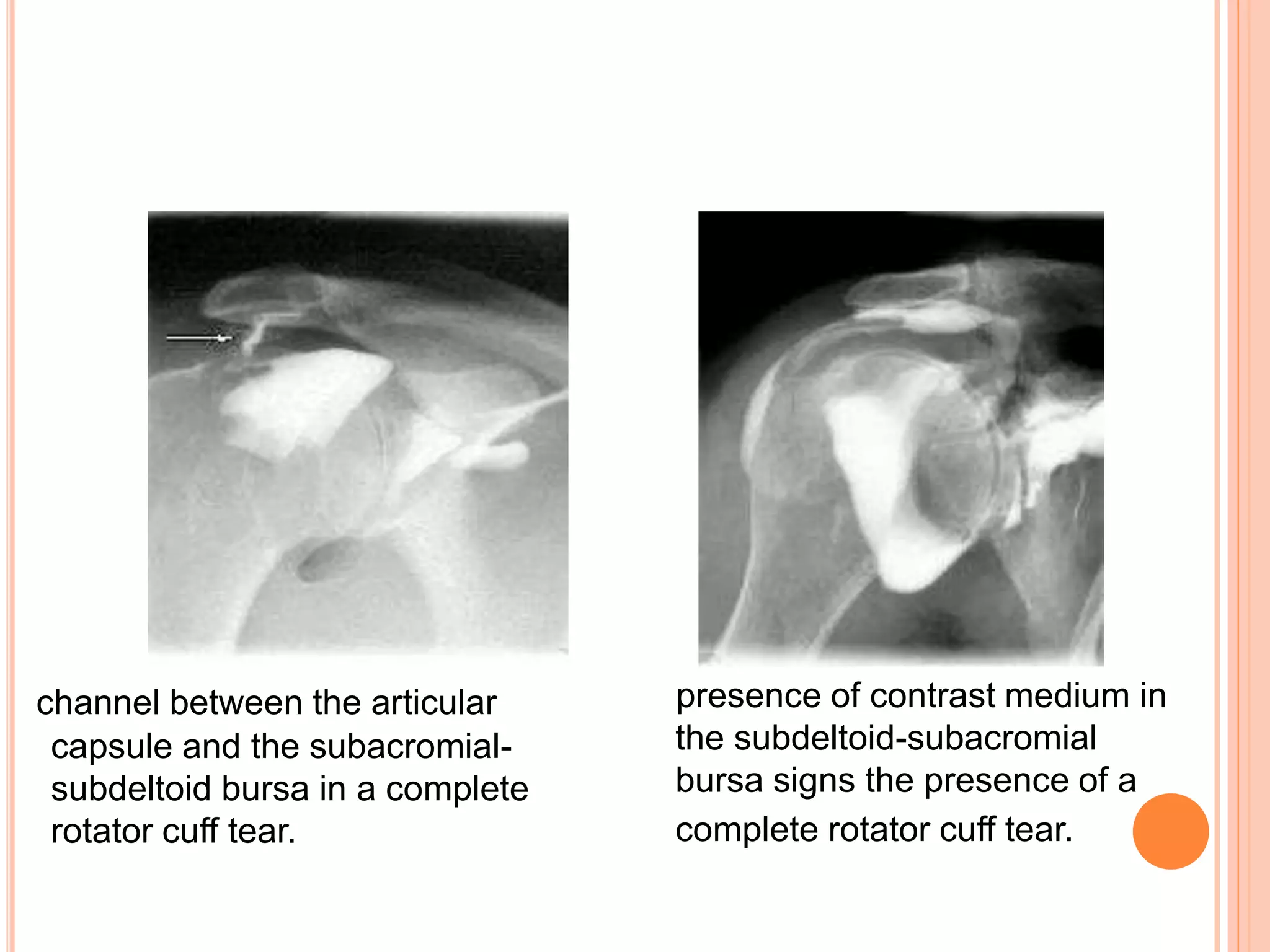
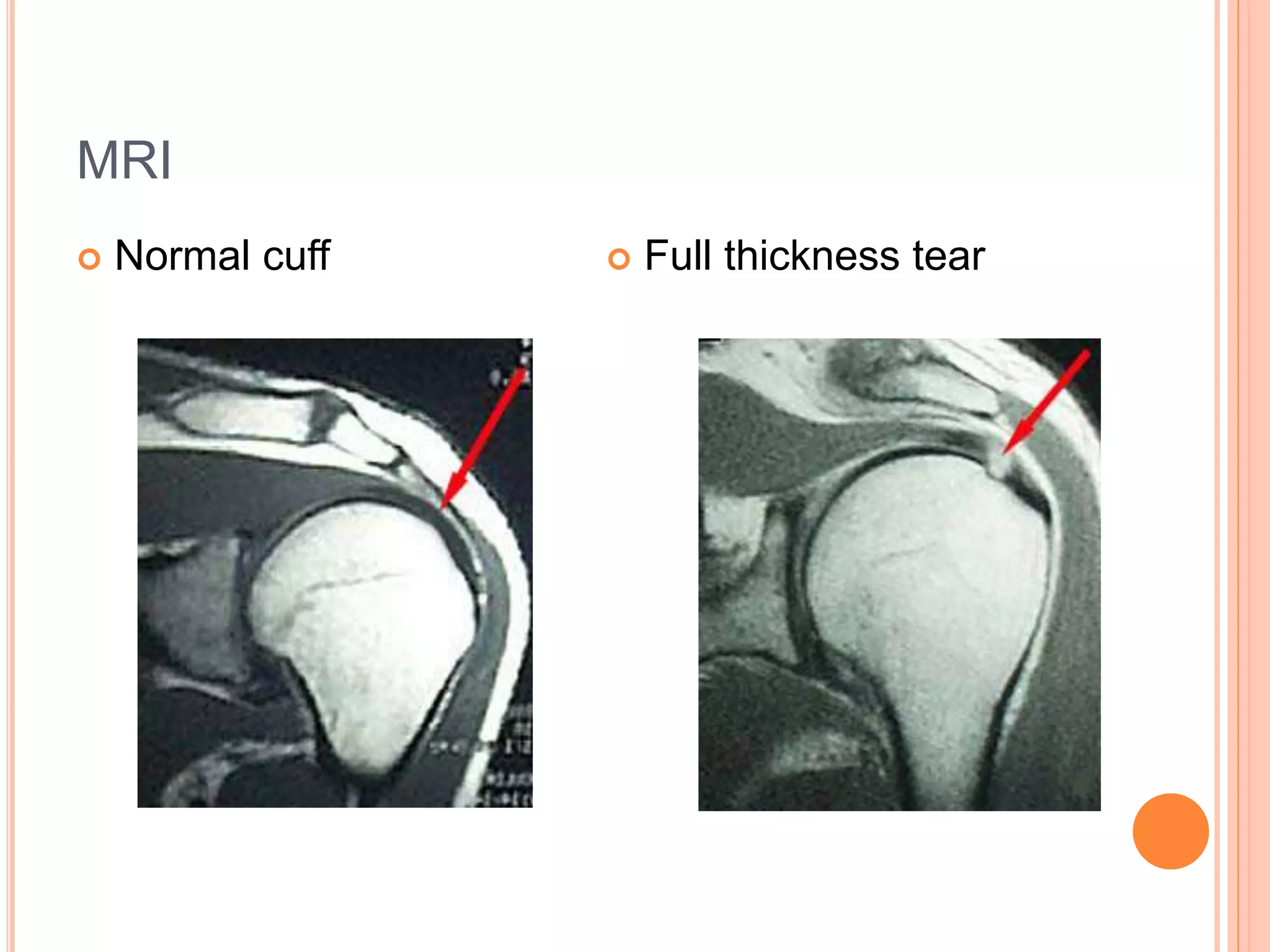
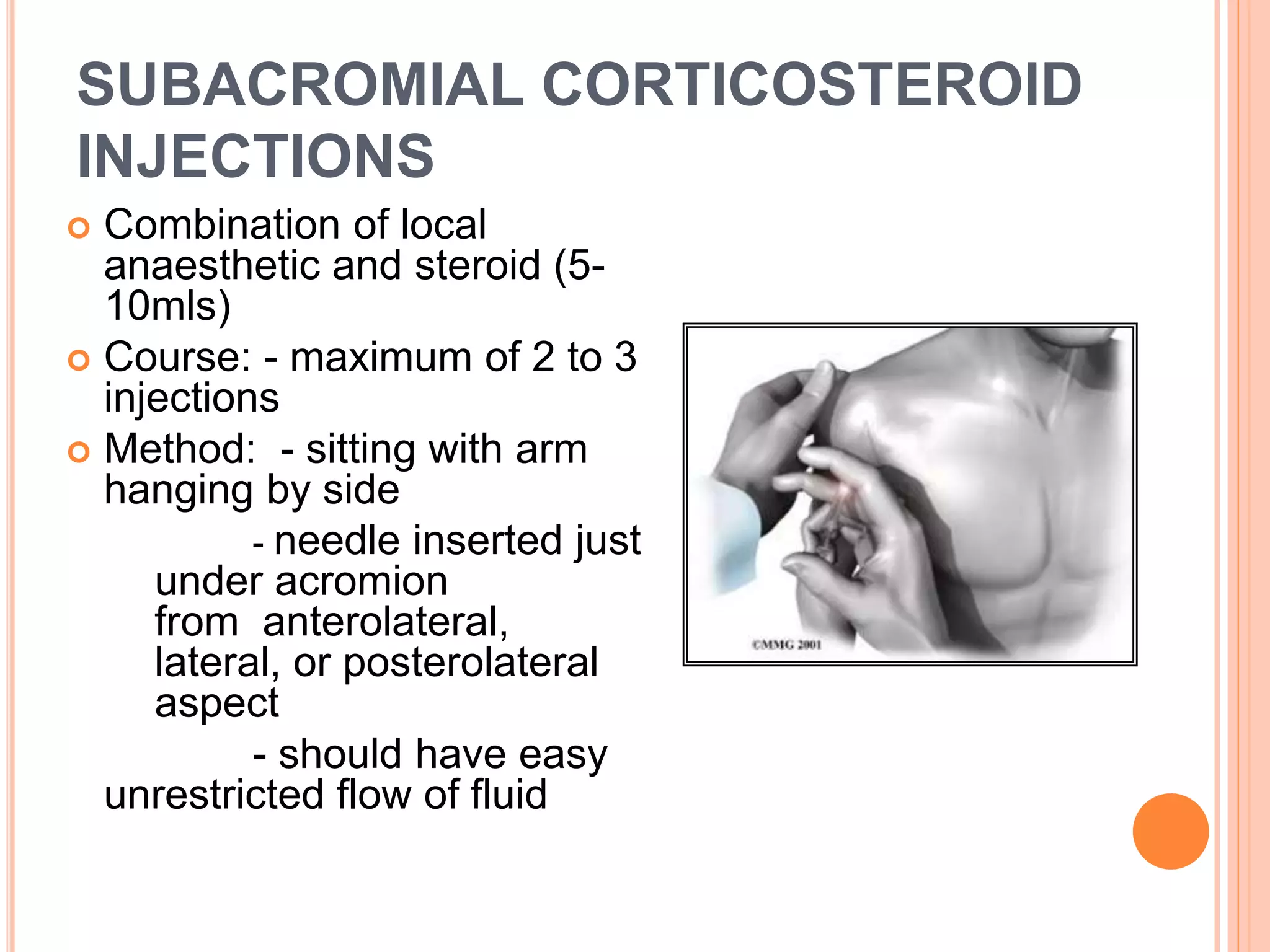
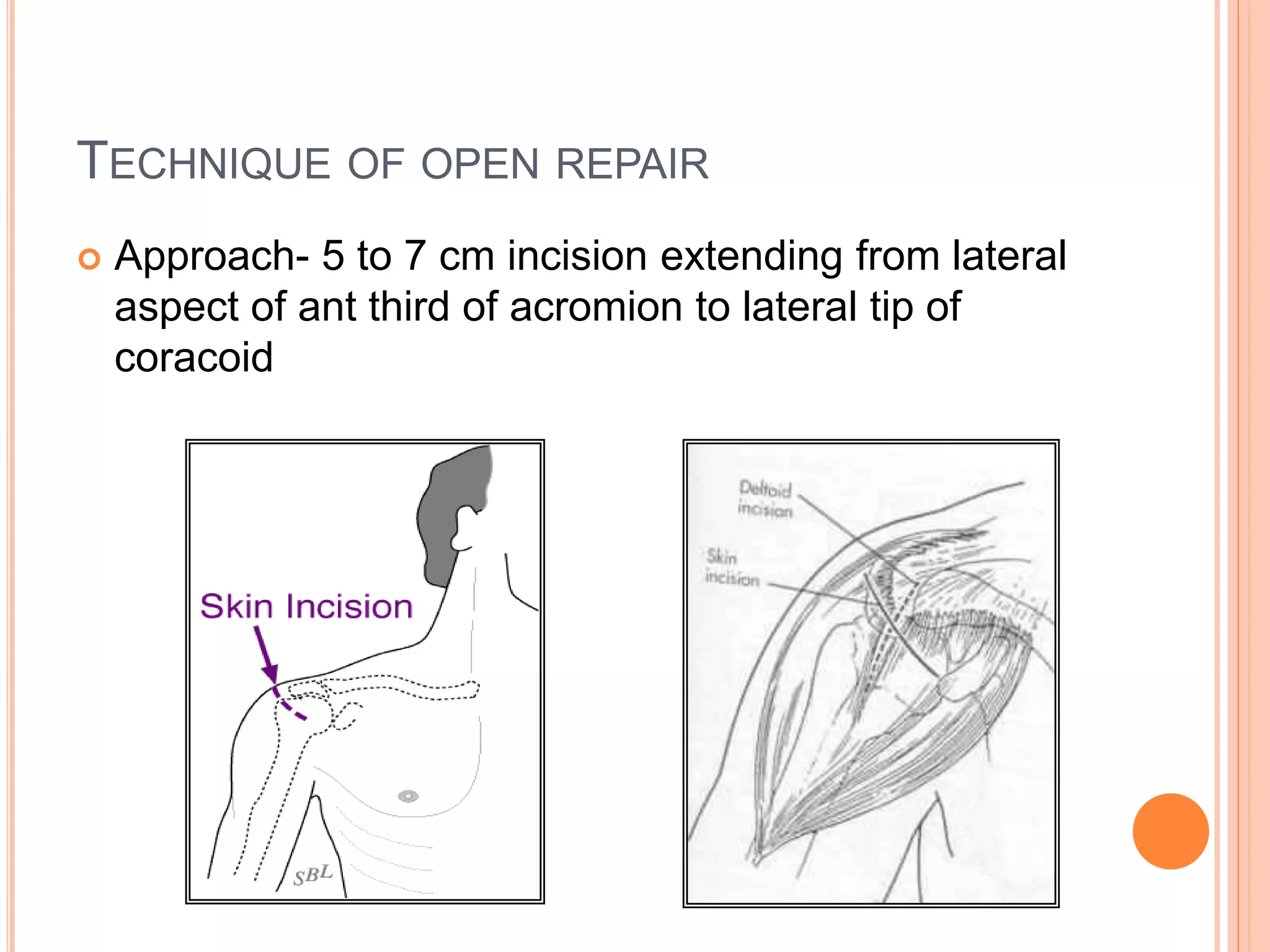
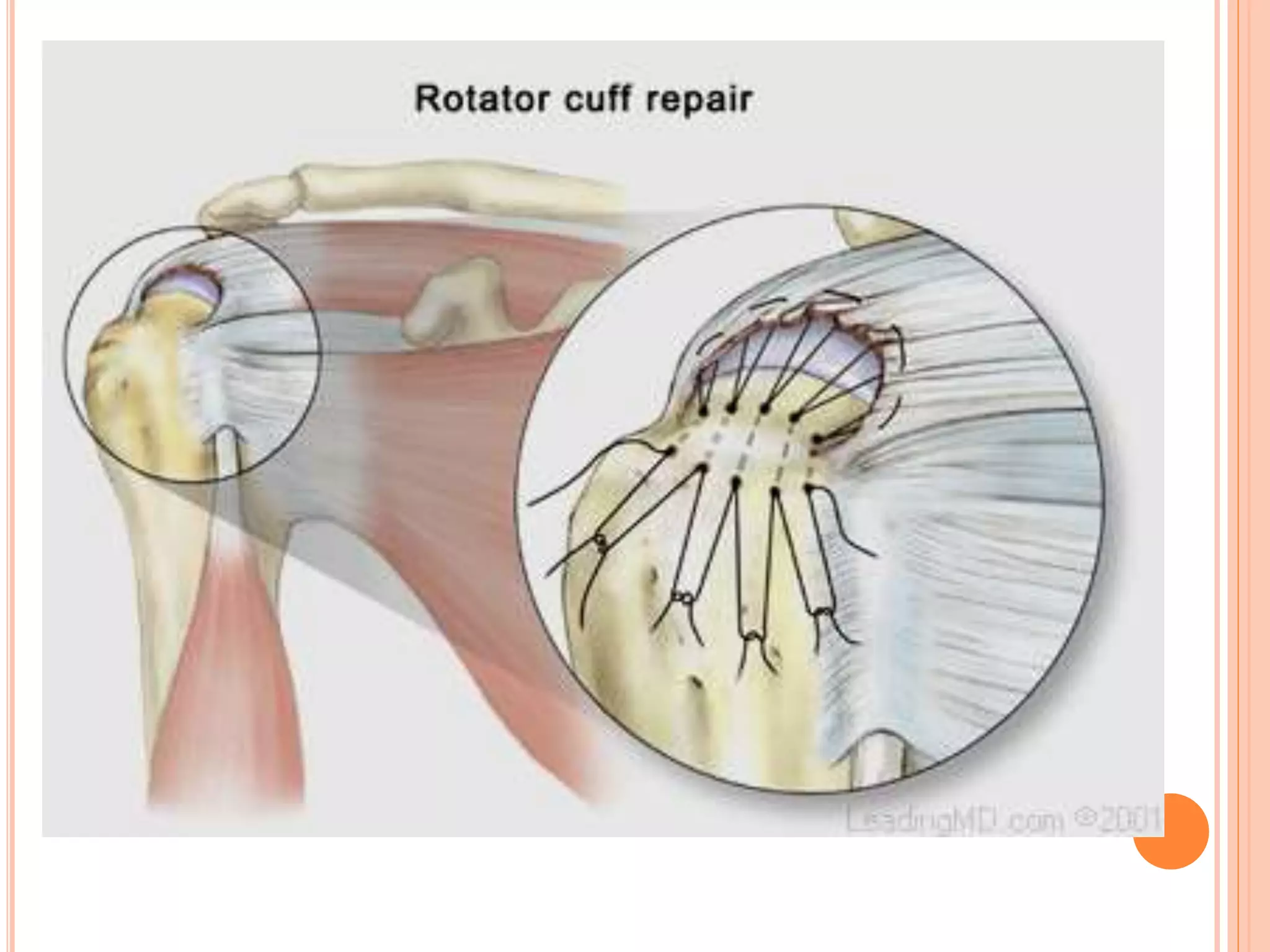
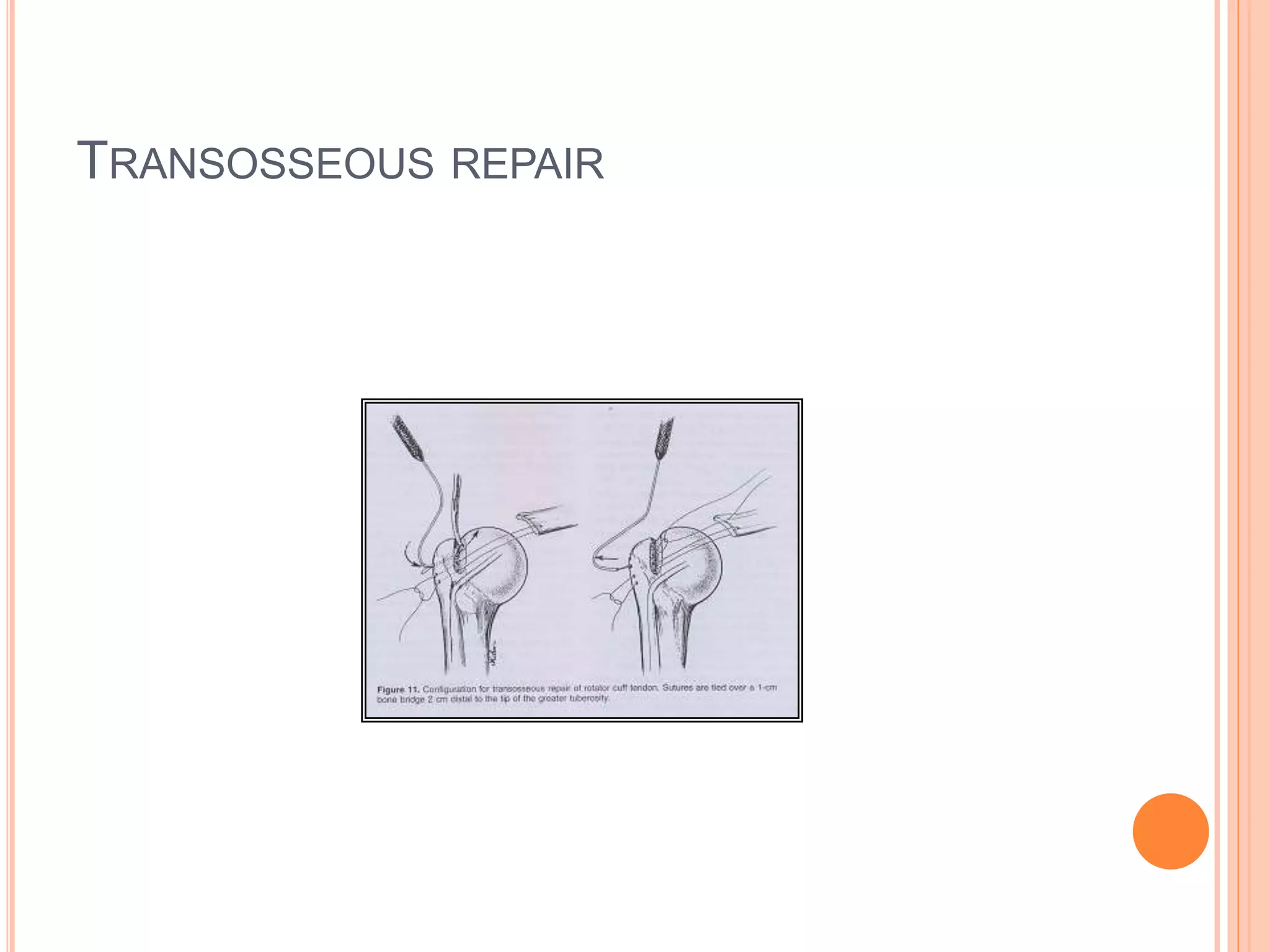
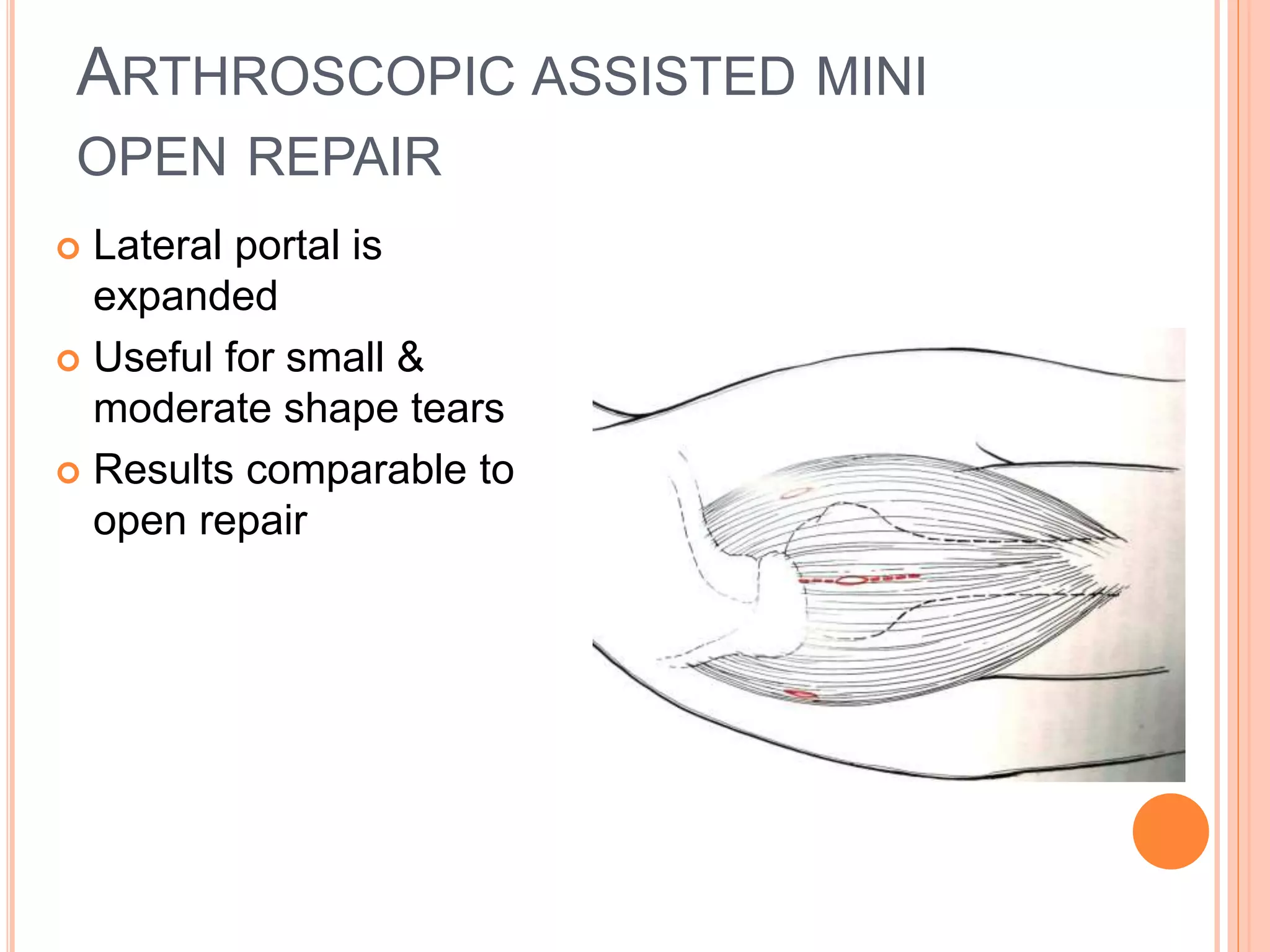
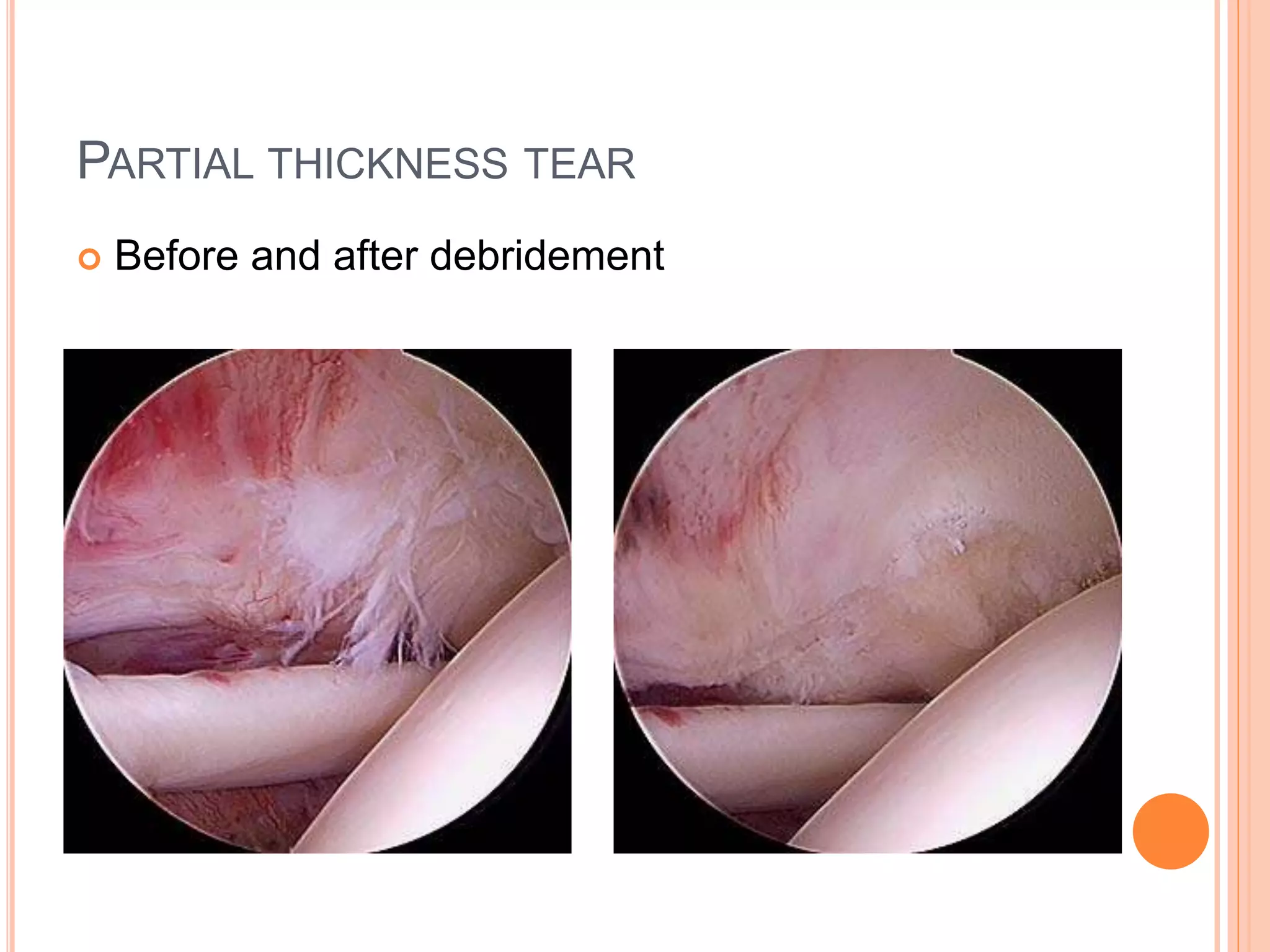
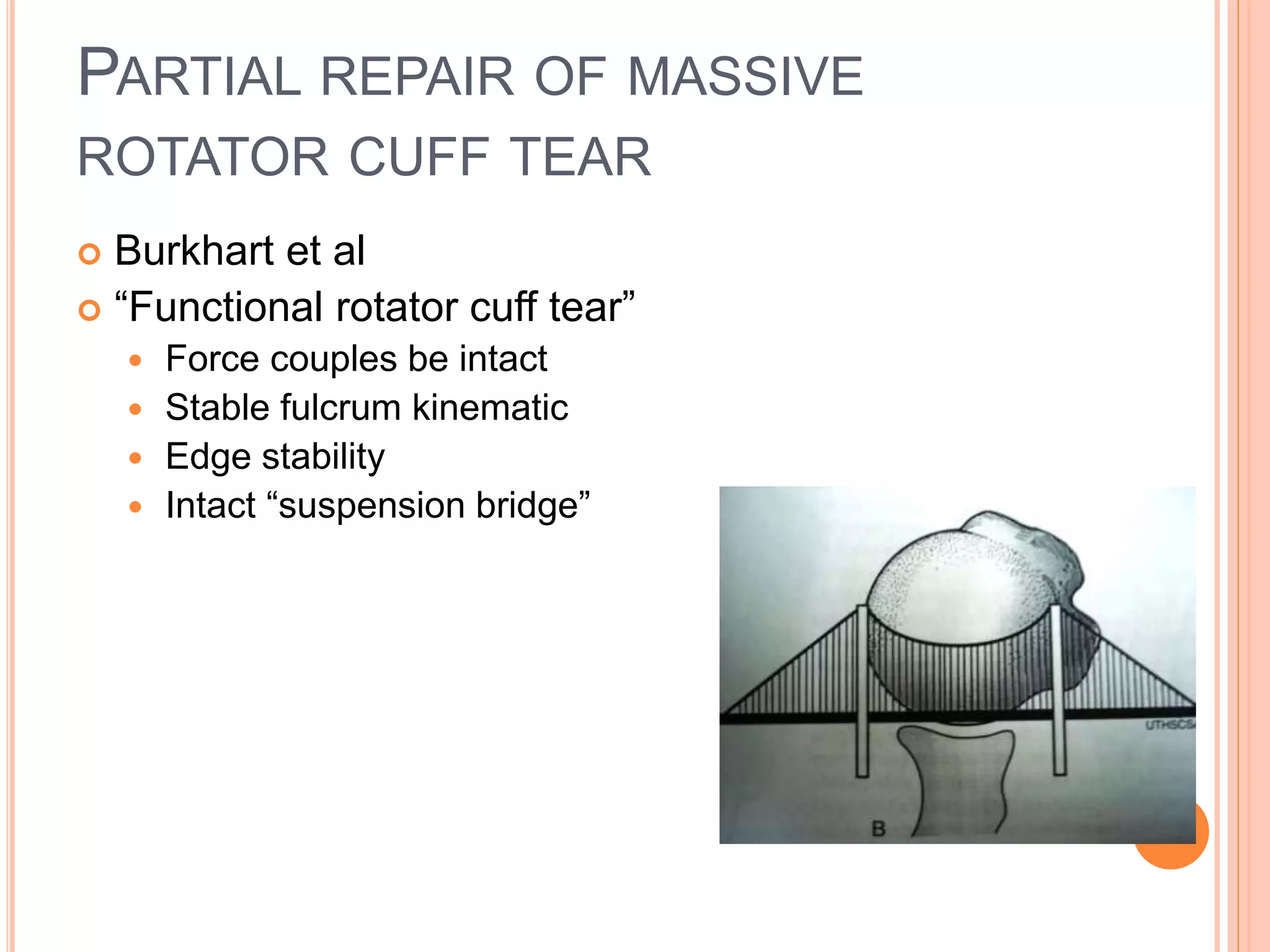
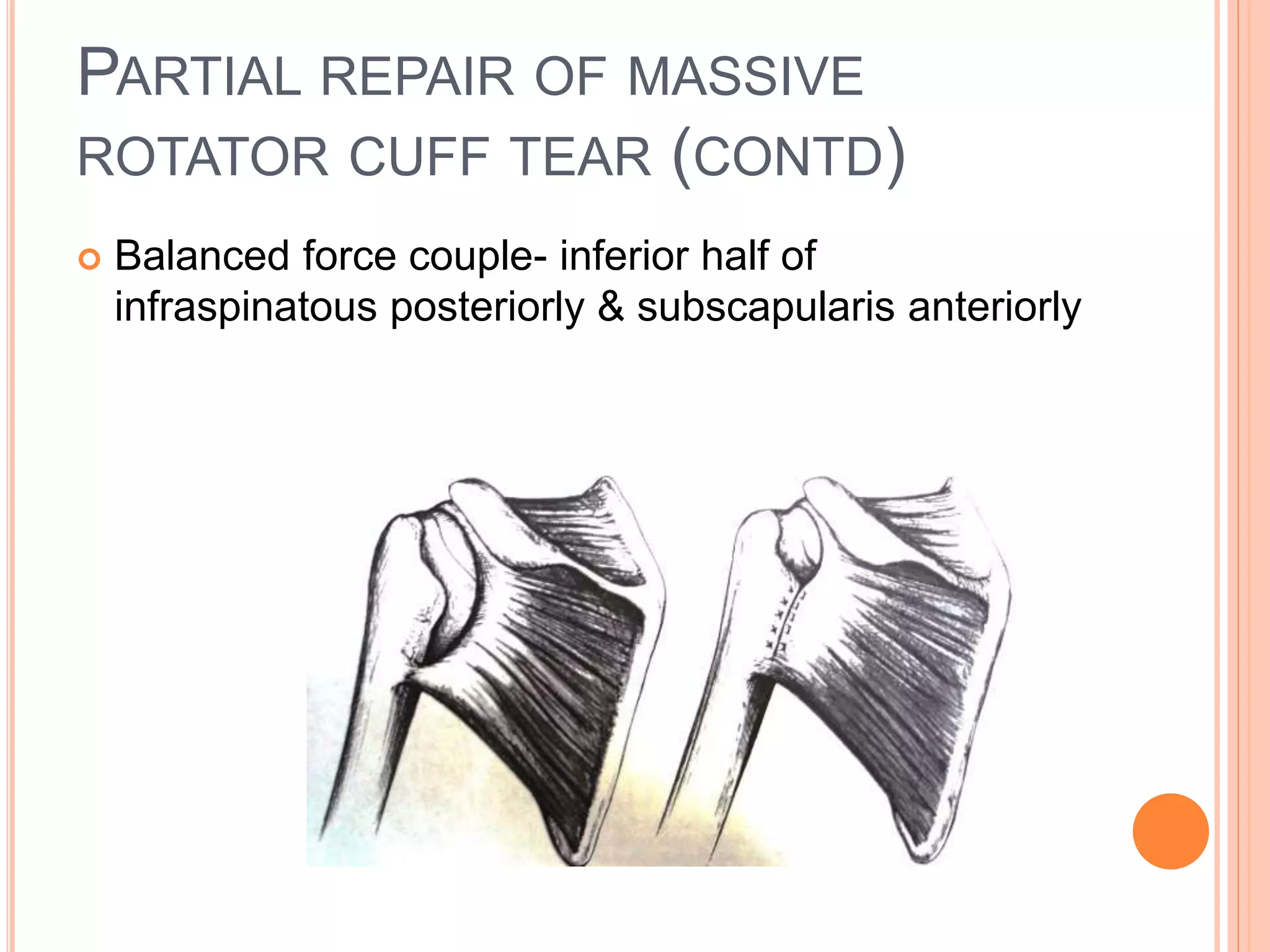
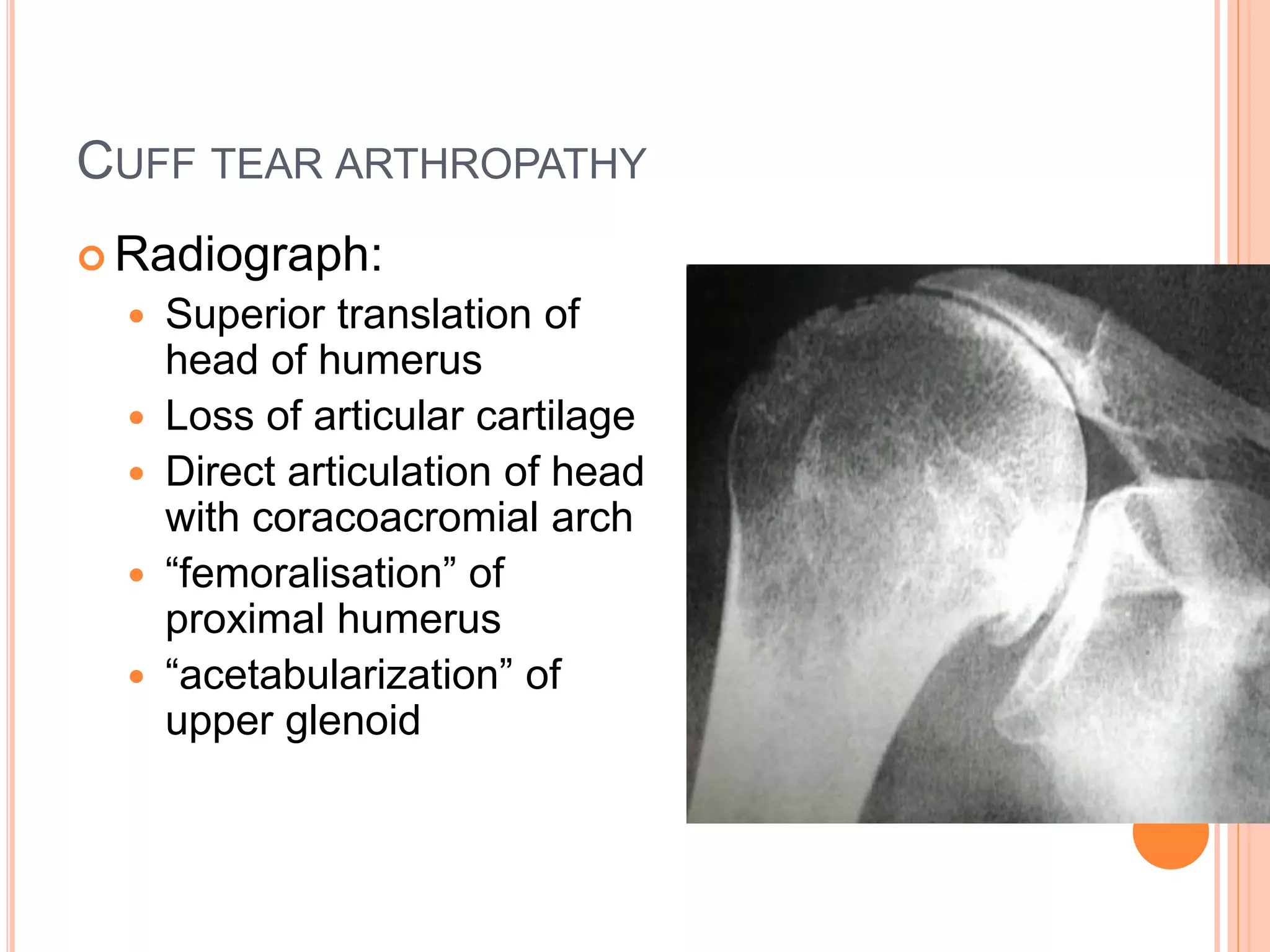
This document provides a review of rotator cuff tears, including their anatomy, function, pathophysiology, clinical presentation, diagnostic tests, differential diagnosis, imaging, and treatment options. It describes the rotator cuff muscles and their role in stabilizing the shoulder joint. Common causes of tears include repeated impingement against bony structures or age-related degeneration. Clinical exams aim to isolate each muscle while imaging such as MRI can determine the size and location of tears. Conservative treatment includes corticosteroid injections and physical therapy, while surgical repair is considered for larger or symptomatic tears.