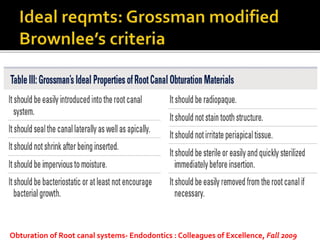
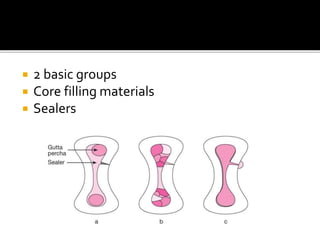
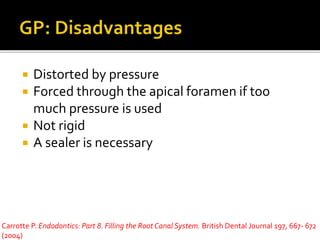
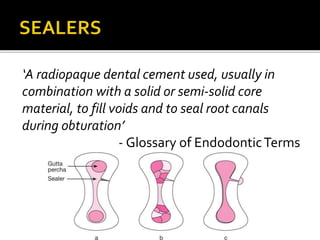
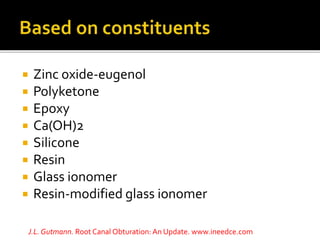
This document discusses the properties and functions of endodontic sealers used during root canal obturation. It provides a list of ideal characteristics for a sealer, including that it should adhere well to root canal walls and gutta percha to form a hermetic seal, be radiopaque, not shrink or leak toxic components, and have antibacterial properties without high toxicity. The sealer functions to fill irregularities and form a fluid-tight seal within the root canal system when used along with a core filling material like gutta percha.