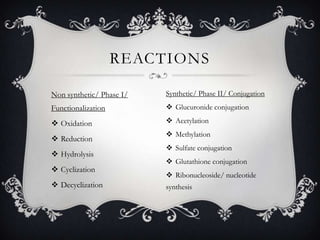
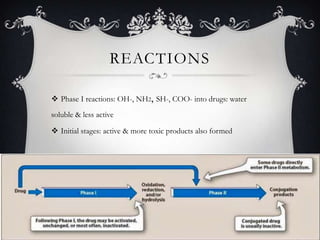
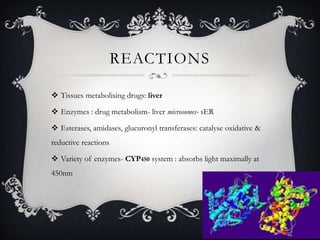
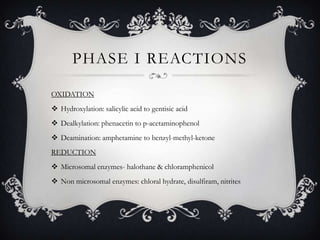
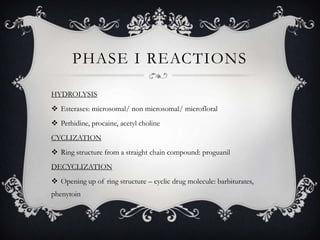
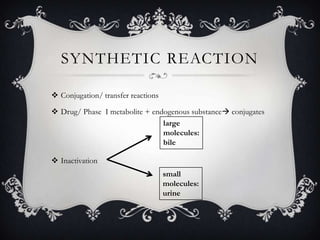
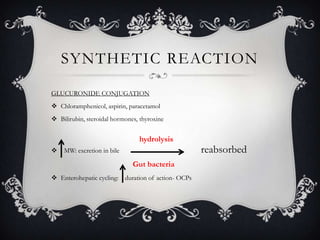
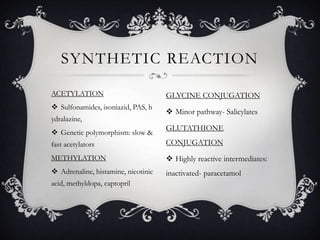
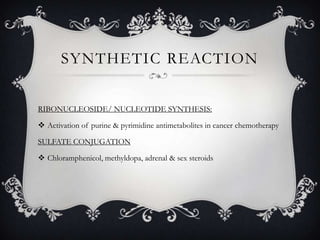
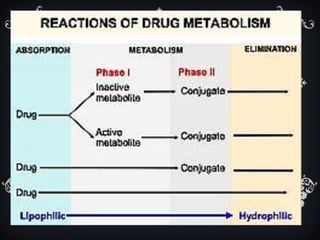
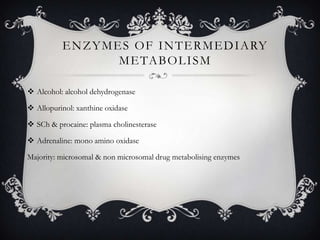
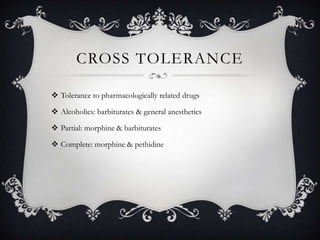
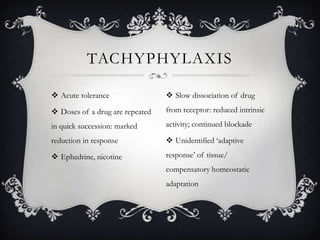
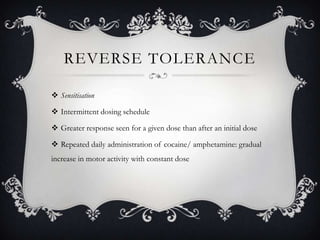
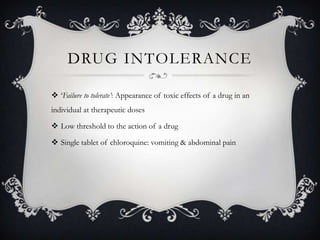
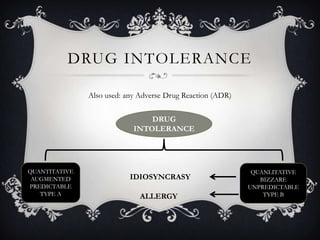
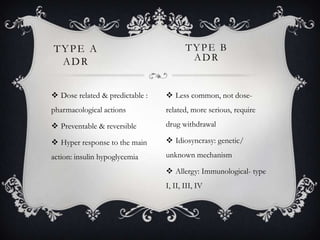
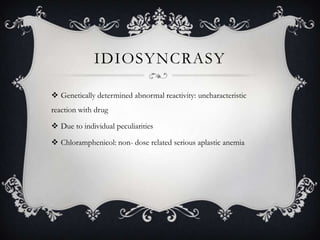
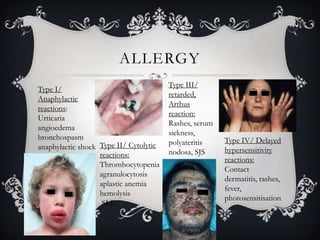
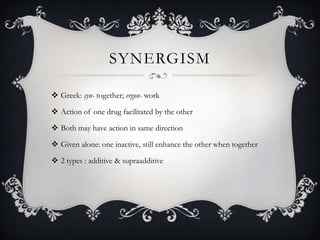
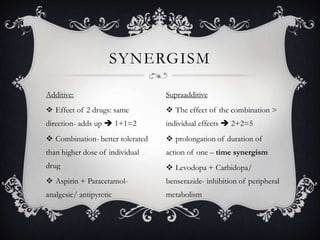
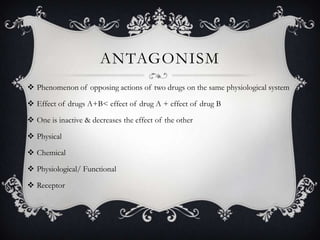
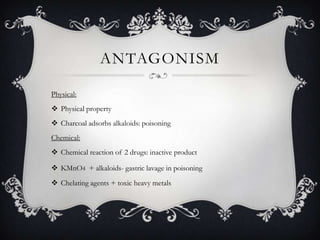
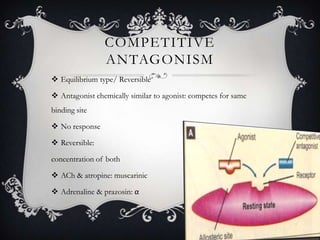
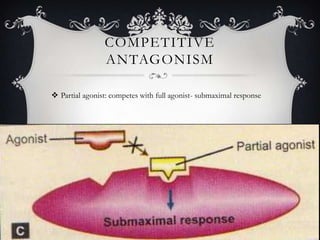
This document discusses various concepts related to pharmacology including the fate of drugs in the body, drug metabolism, tolerance, intolerance, synergism, and antagonism. It provides details on the three main fates of drugs after absorption which are metabolic transformation, spontaneous chemical changes, and excretion unchanged. It also describes the two phases of drug metabolism and various metabolic reactions including conjugation. Factors affecting drug metabolism and development of tolerance are summarized. The mechanisms and types of tolerance, intolerance, synergism, antagonism, and cumulative effects are defined.