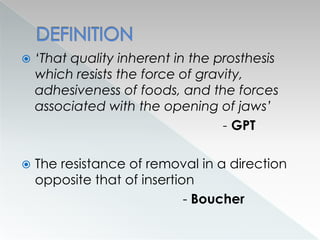
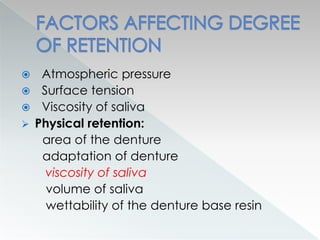
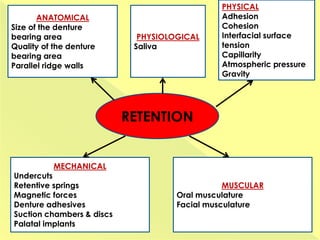
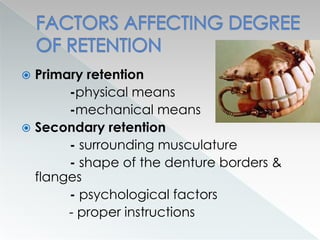
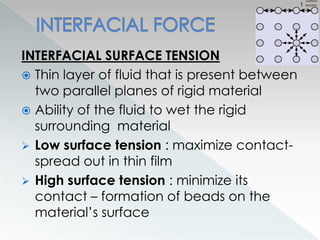
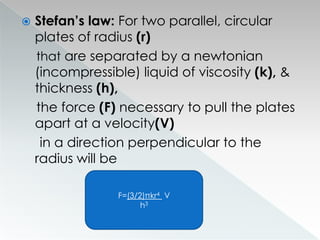
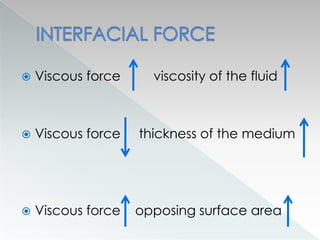
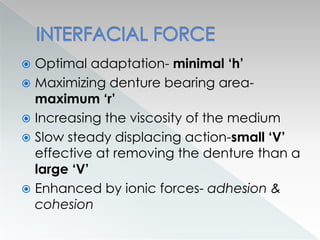
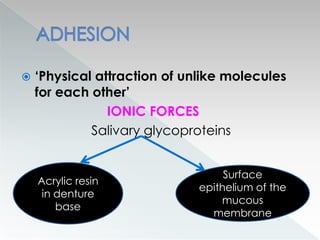
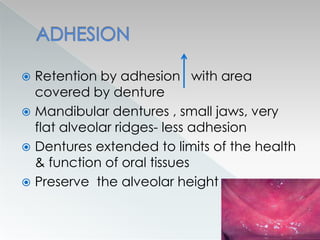
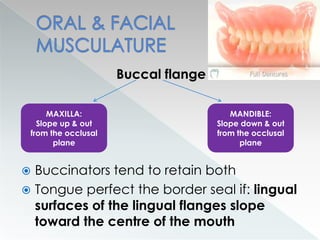
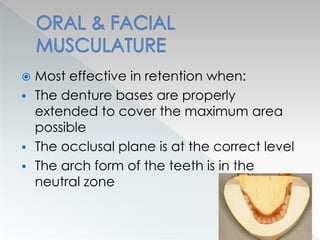
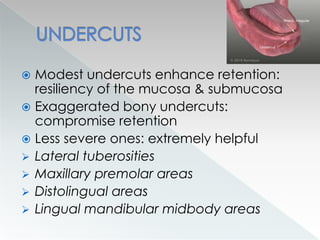
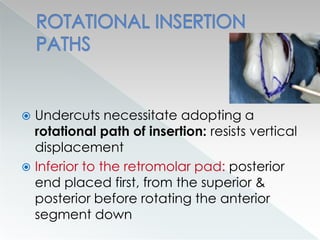
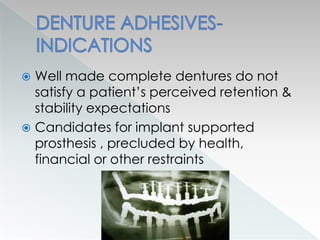
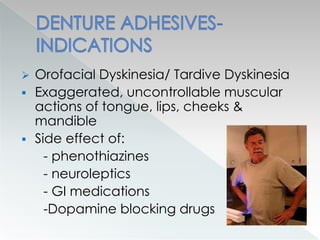
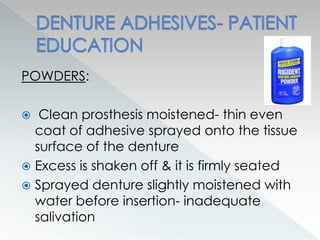
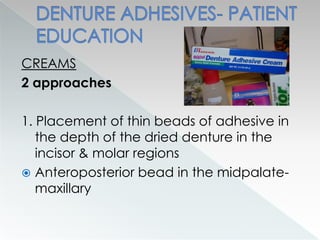
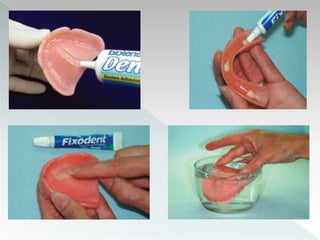
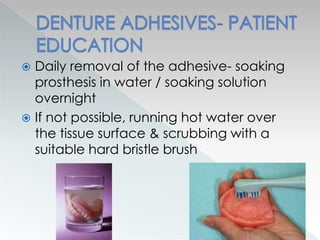
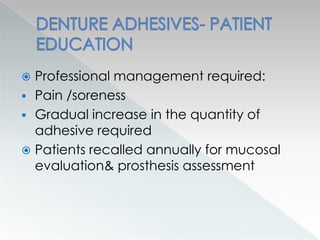
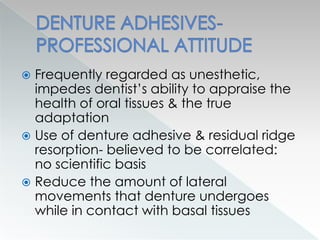
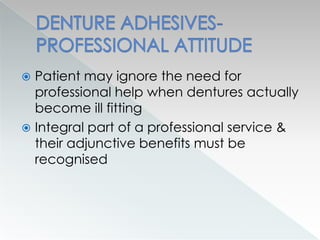
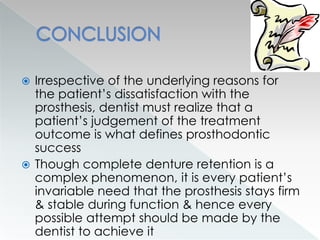
This document discusses factors affecting denture retention, including classification, interfacial forces, adhesion, cohesion, oral and facial musculature, atmospheric pressure, undercuts, parallel walls, and gravity. It defines retention as the resistance of a denture to forces that attempt to displace it from its basal seat. Primary retention comes from physical and mechanical means like surface area, adaptation, viscosity and secondary retention from surrounding musculature. Denture adhesives are discussed as a way to augment existing retention mechanisms by increasing adhesion, cohesion and viscosity between the denture and mucosa.