The document discusses the monoblock obturation technique in root canal treatment, emphasizing the necessity for proper sealing and bonding to eliminate microbial presence effectively. It critiques gutta-percha as an obturation material, outlining its shortcomings like poor adhesion and limited robustness, while presenting advancements such as bioactive materials and resin-based systems. Ultimately, it highlights that current materials lack the necessary elastic properties for effective dental reinforcement and that successful monoblock configurations face challenges in achieving both strong bonding and sealing capabilities.















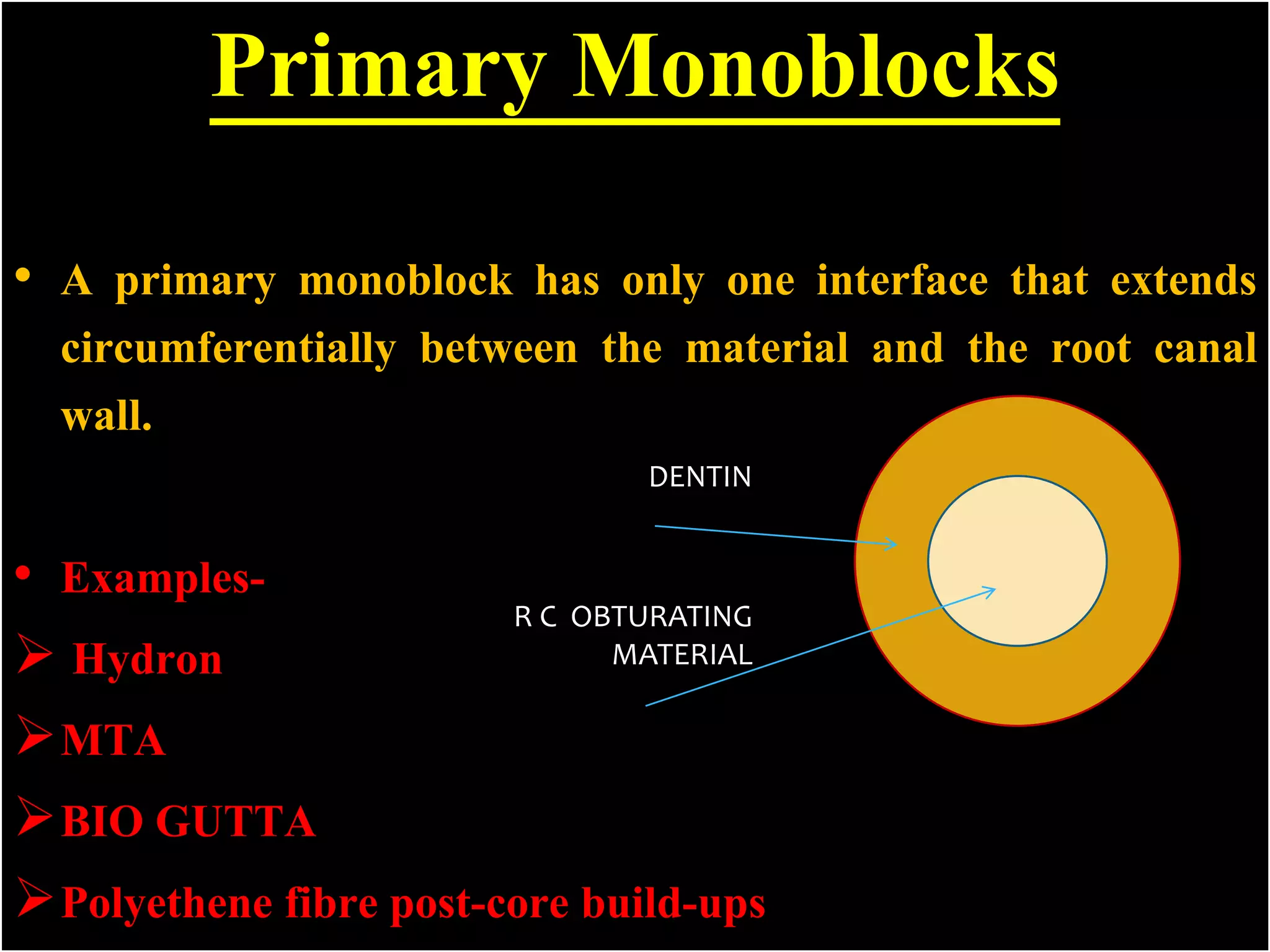











![1-The first generation;
contained poly [2-hydroxyethylmethacrylate] HEMA as major
ingredient was marketed as Hydron.
2-The second generation:
are hydrophilic and does not require etching to the adjunctive use of
a dentin adhesive Eg; ENDOREZ.
3-The third generation :
involve the use of a self-etching primer and dual-cured resin
composite Sealer Eg; RESILON/EPIPHANY.
4-The fourth generation sealers:
where in the etchant, primer and sealer were incorporated into an
all-in-one self-etching, self-adhesive sealer Eg; METASEAL.](https://image.slidesharecdn.com/monoblockbb2vv-170607090143/75/dental-Monoblock-obturation-technique-or-concept-in-endodontics-29-2048.jpg)




































