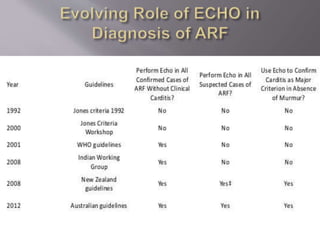
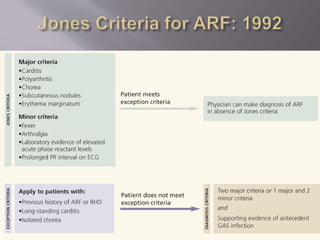
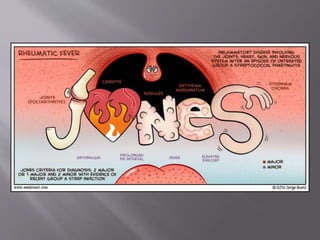
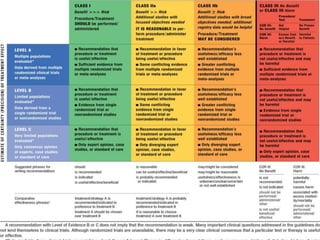
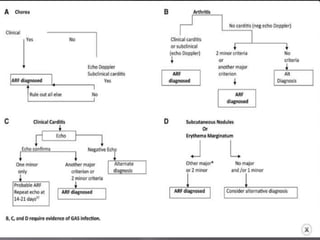
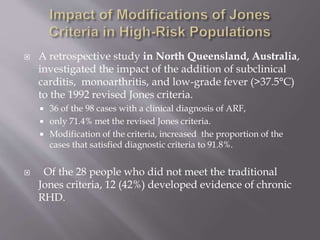
The document discusses the decline in the incidence of Acute Rheumatic Fever (ARF) over several decades, highlighting its continued impact on socially and economically disadvantaged populations. It emphasizes the need for tailored diagnostic criteria and the use of echocardiography in identifying valvular changes in suspected ARF cases. Additionally, modifications to the Jones criteria are suggested to improve diagnostic sensitivity, particularly in higher-risk groups.