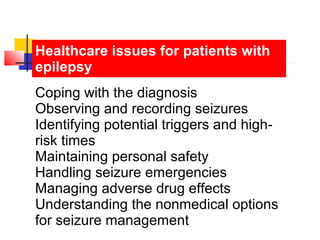
This document discusses epilepsy, including its definition, types, diagnostic workup, treatment, and management. The key points are:
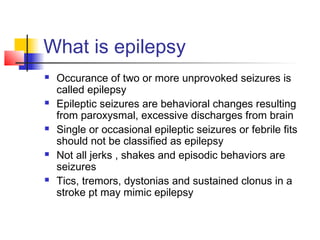
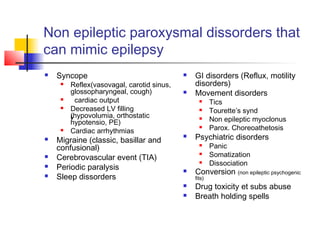
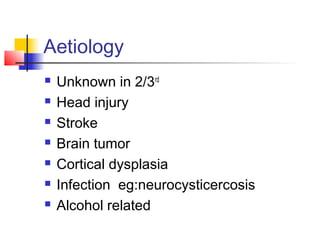
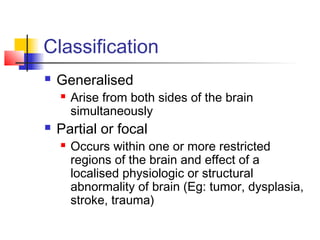
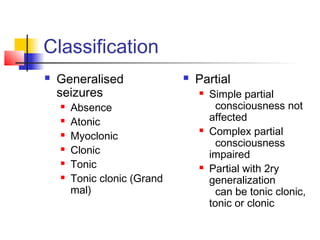
1. Epilepsy is defined as two or more unprovoked seizures and results from excessive neuronal discharges in the brain. Seizures can be generalized, arising from both sides of the brain simultaneously, or partial/focal, arising from a localized region.
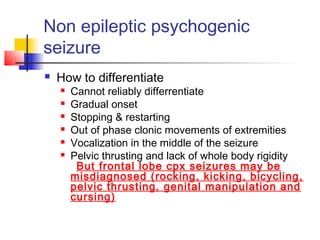
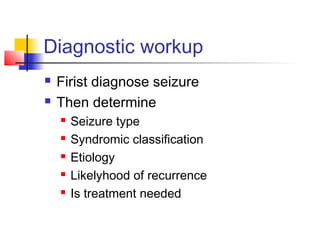
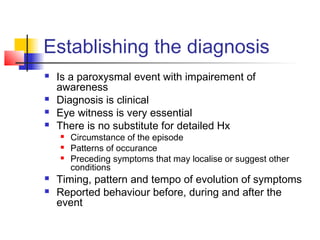
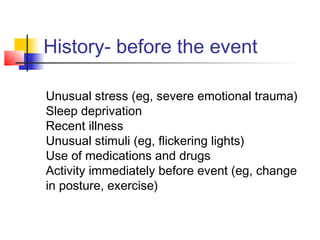
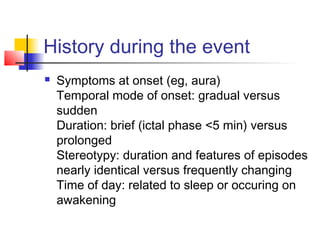
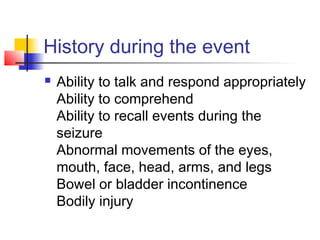
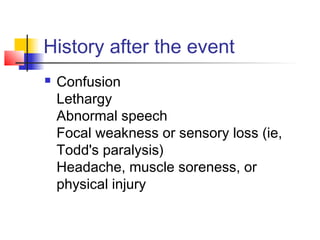
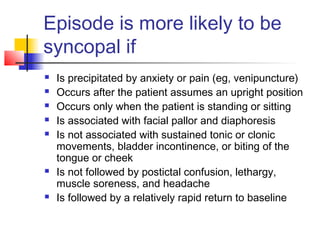
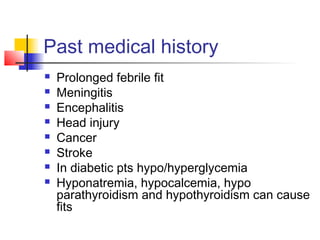
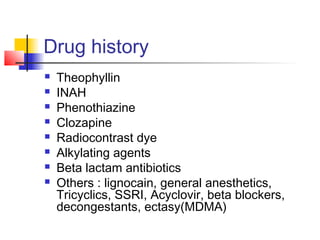
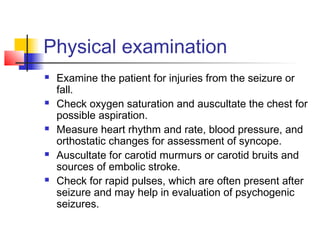
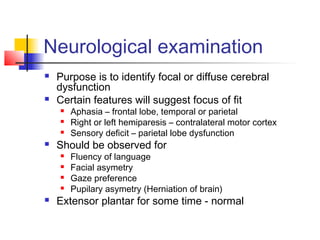
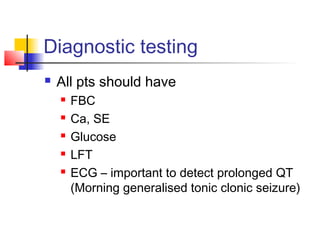
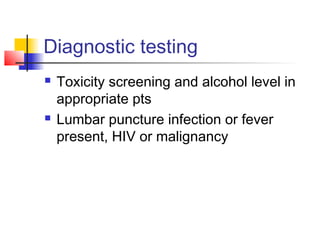
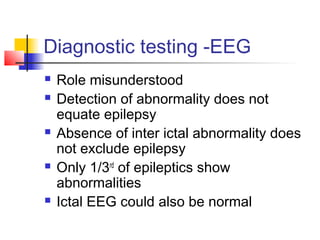
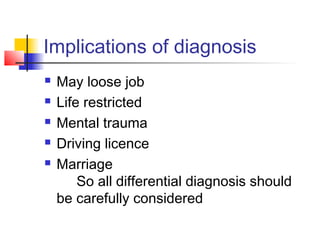
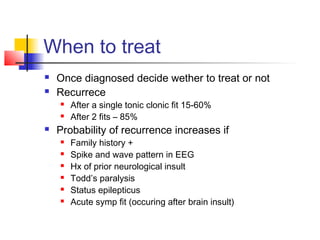
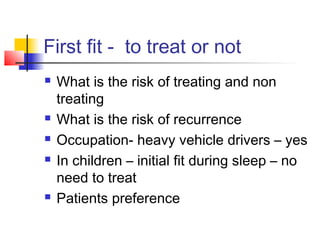
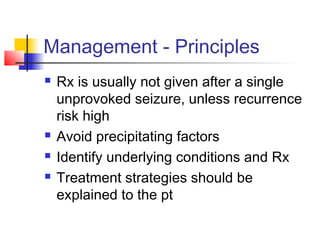
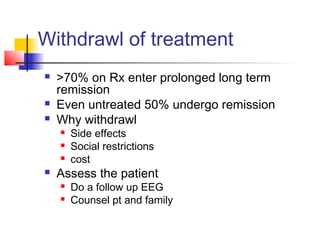
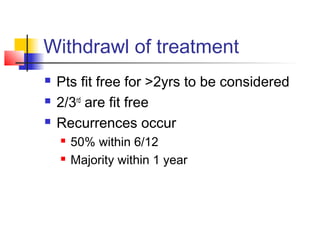
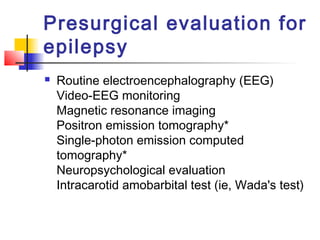
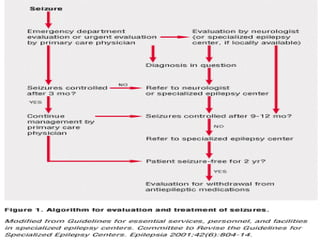
2. The diagnostic workup involves a detailed history, physical exam, neurological exam, EEG, imaging studies, and lab tests to determine seizure type, etiology, and likelihood of recurrence to guide treatment decisions.
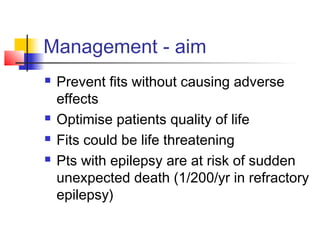
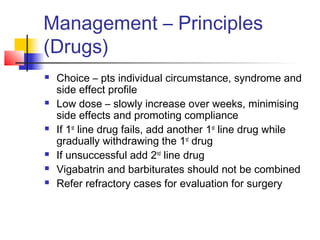
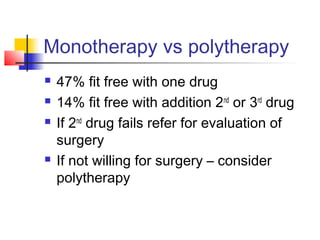
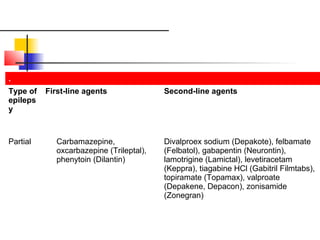
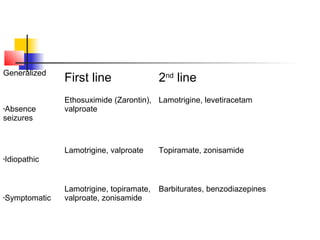
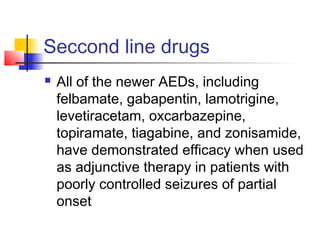
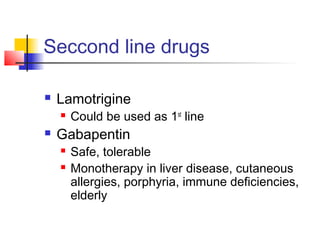
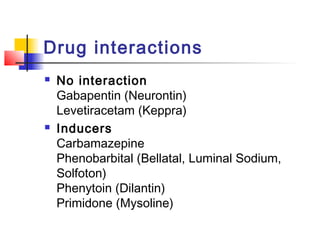
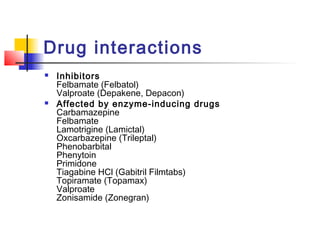
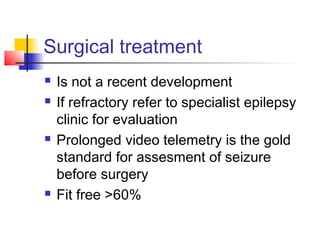
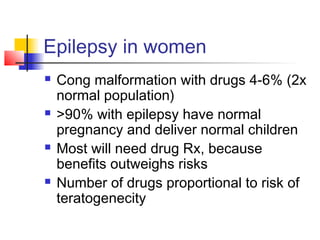
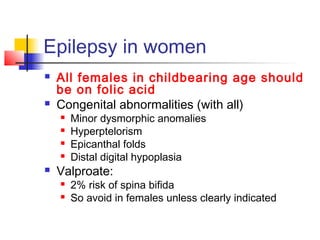
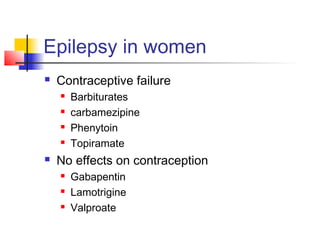
3. Treatment aims to prevent seizures without adverse effects and improve quality of life. First-line treatments