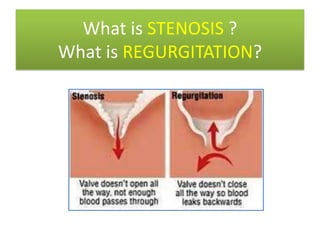
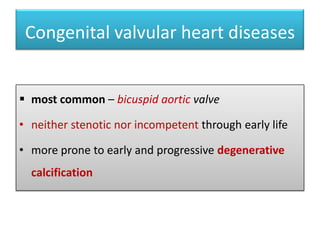
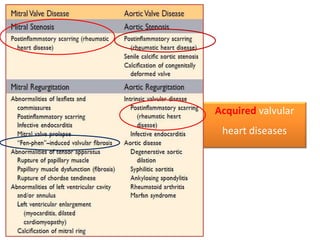
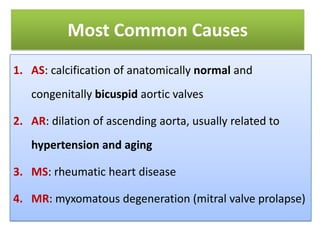
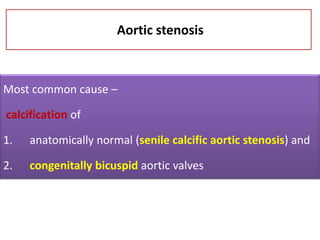
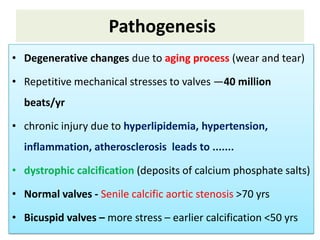
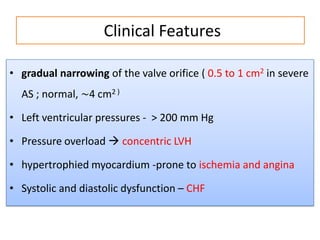
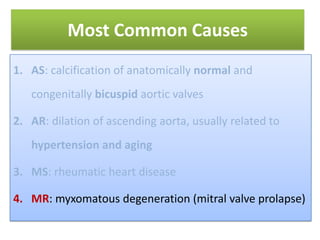
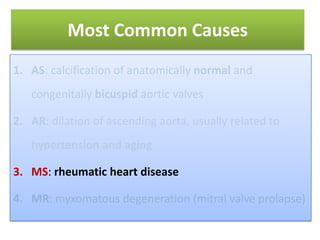
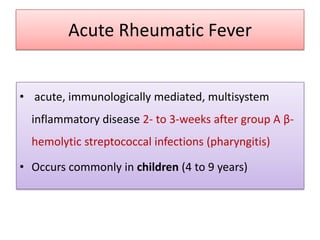
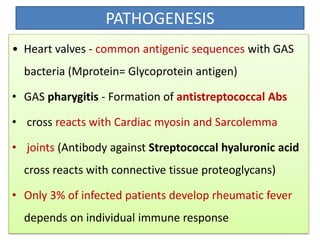
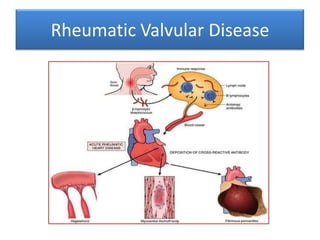
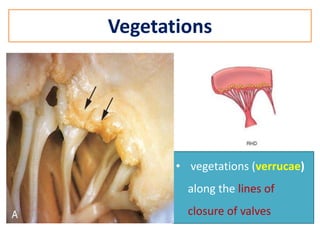
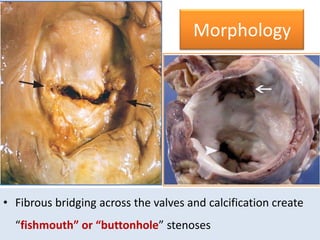
Valvular heart disease refers to pathological conditions affecting the heart valves. The two main types are stenosis, which is a failure of a valve to open completely, and regurgitation, which is a failure of a valve to close completely. Valvular heart diseases can be either congenital or acquired later in life. Rheumatic heart disease is a major acquired cause, resulting from rheumatic fever following a streptococcal throat infection, and often leads to mitral stenosis over time due to scarring. Calcific aortic stenosis is also common, usually due to age-related degeneration and calcium buildup on the aortic valve.