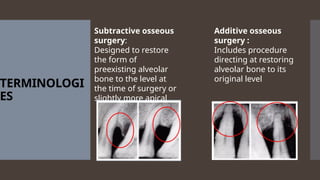
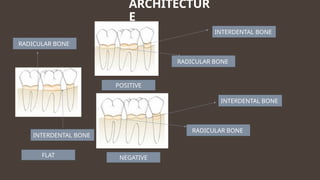
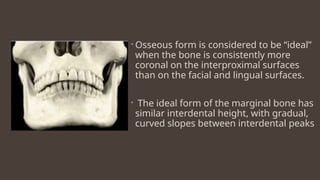
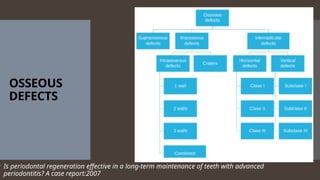
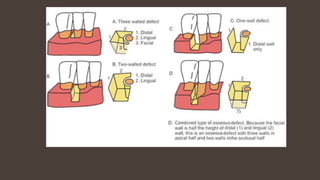
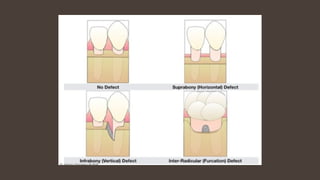
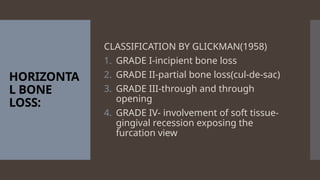
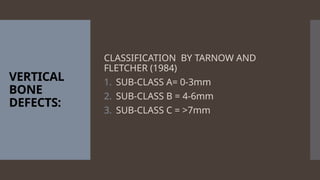
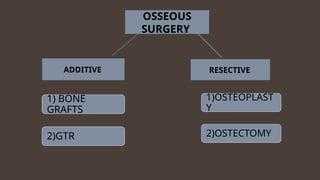
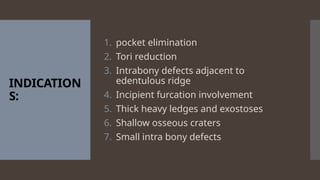
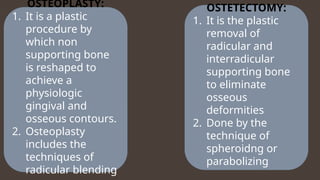
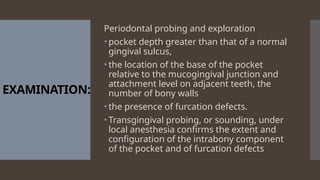
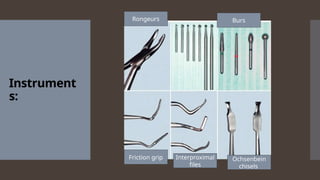
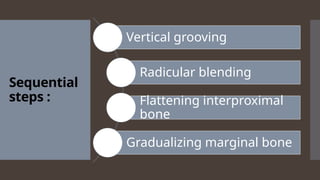
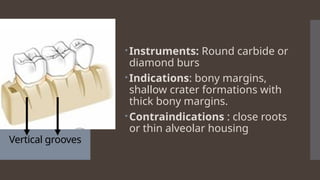
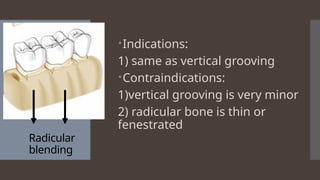
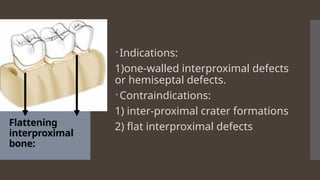
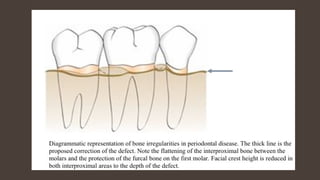
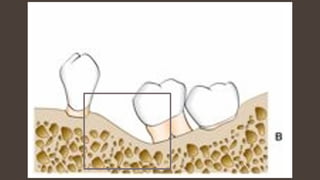
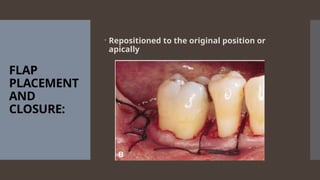
The document discusses resective osseous surgery, its historical background, various techniques, terminology, indications, and contraindications. It emphasizes the importance of reshaping alveolar bone to alleviate periodontal deformities and achieve physiological gingival contours. The conclusion highlights that while not applicable to all bony abnormalities, effective osseous surgery can significantly modify dental defects and improve long-term oral hygiene maintenance.