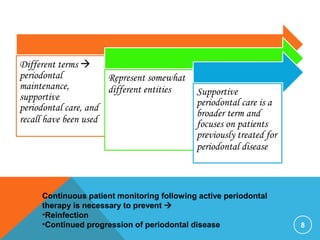
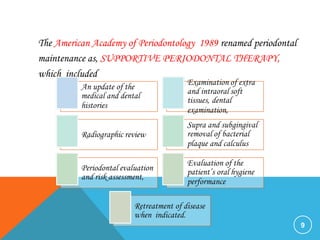
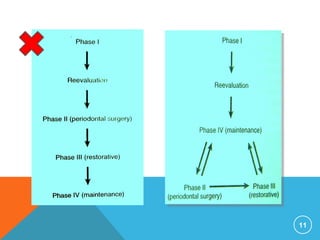
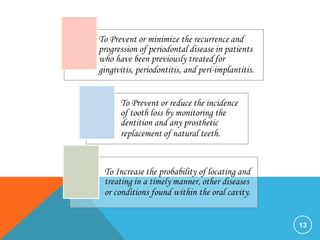
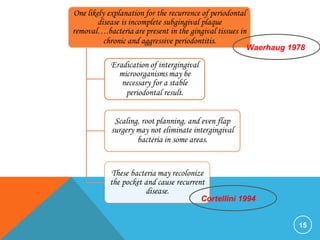
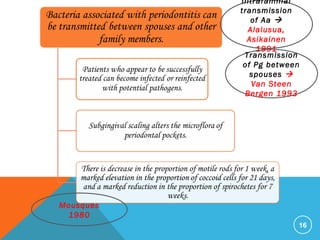
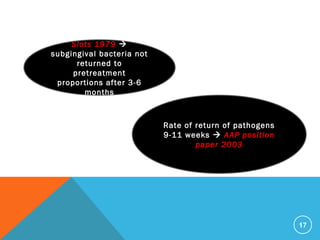
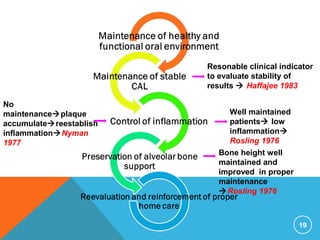
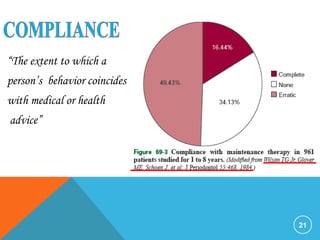
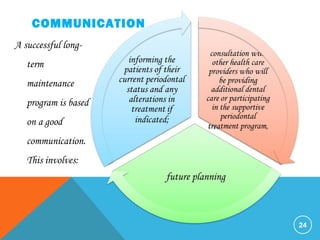
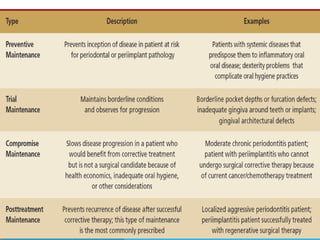
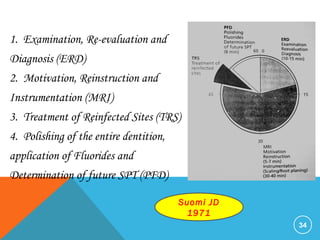
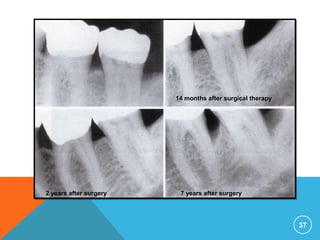
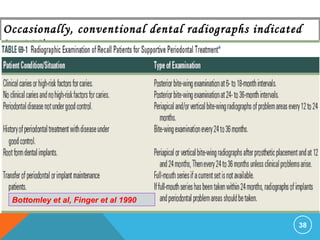
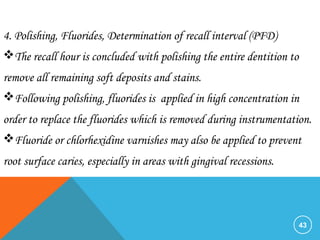
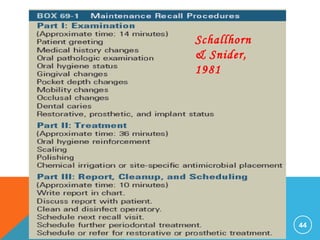
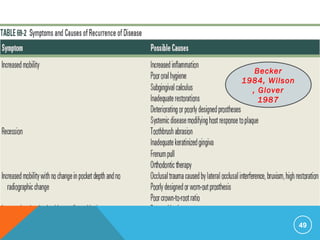
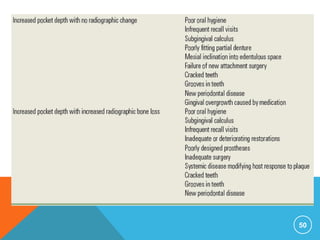
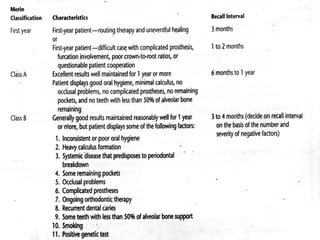
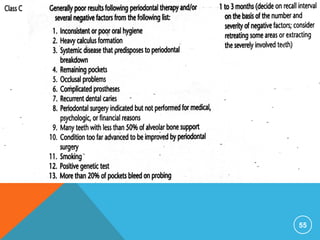
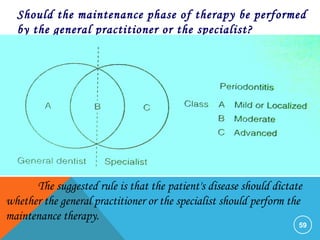
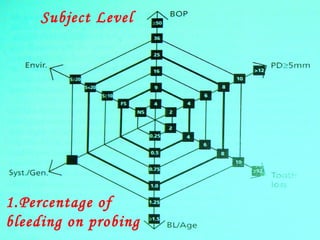
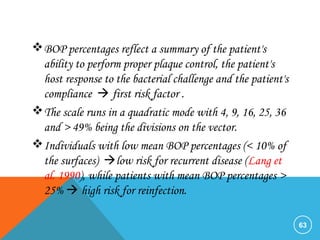
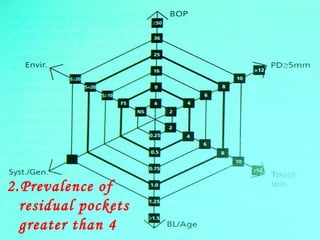
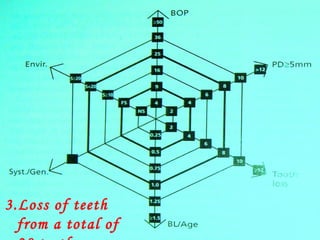
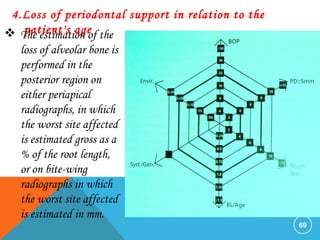
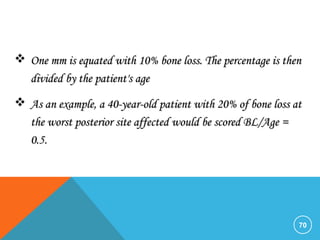
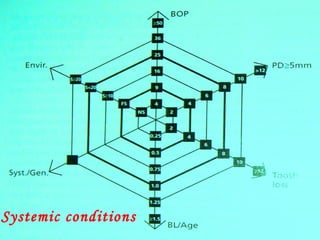
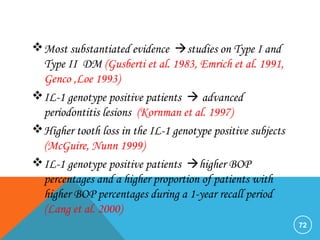
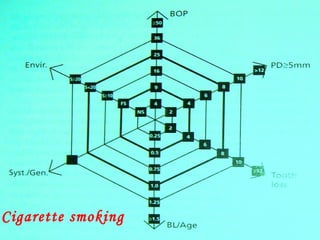
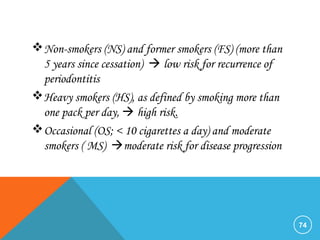
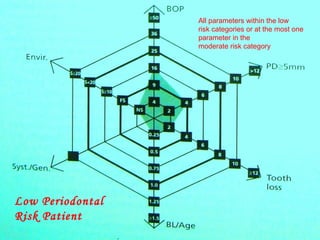
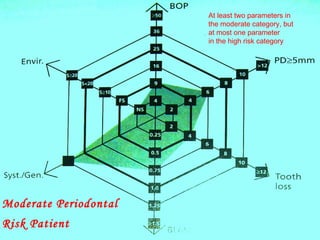
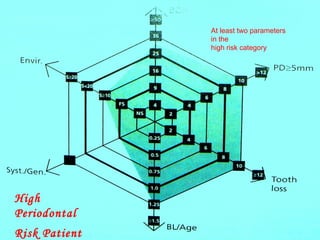
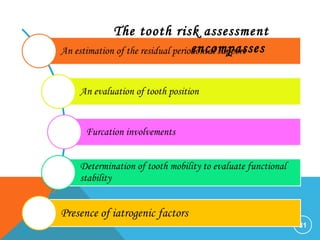
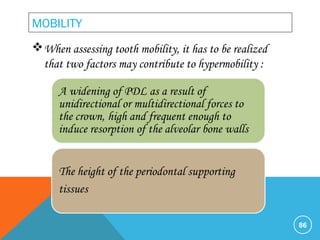
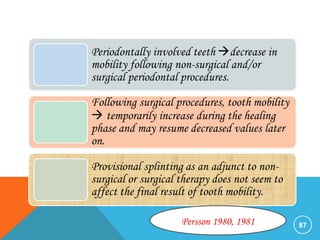
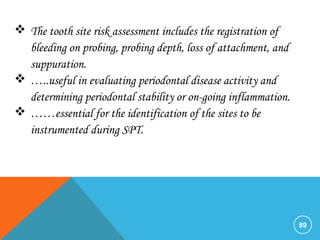
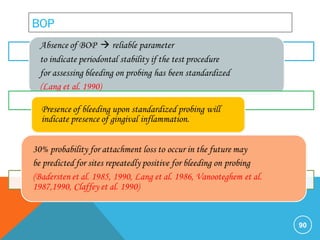
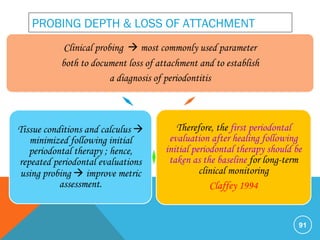
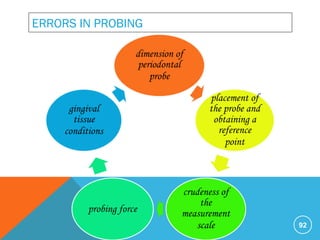
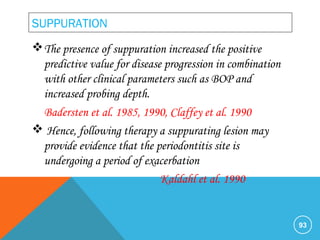
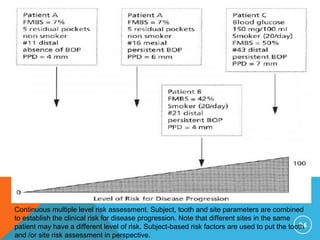
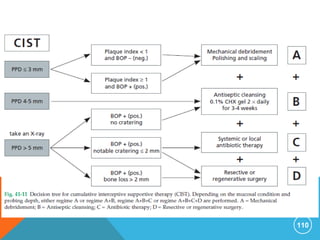
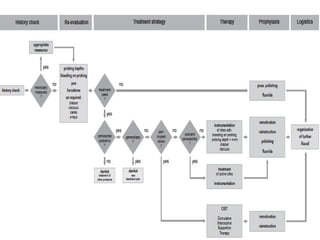
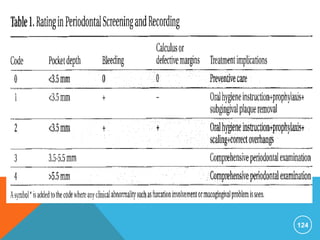
This document discusses supportive periodontal therapy (SPT). It begins with an introduction and overview of SPT. It then discusses the rationale and objectives of SPT, which include preventing disease recurrence and progression. Compliance is important for effective SPT. The document outlines the typical parts of an SPT visit, including examination, motivation and instrumentation, treatment of reinfected sites, and determination of recall interval. Research shows that regular SPT every 3-6 months is effective at preventing further attachment and bone loss. The document also discusses classifying post-treatment patients, referring patients to specialists, assessing risk of disease recurrence, and complications of SPT.