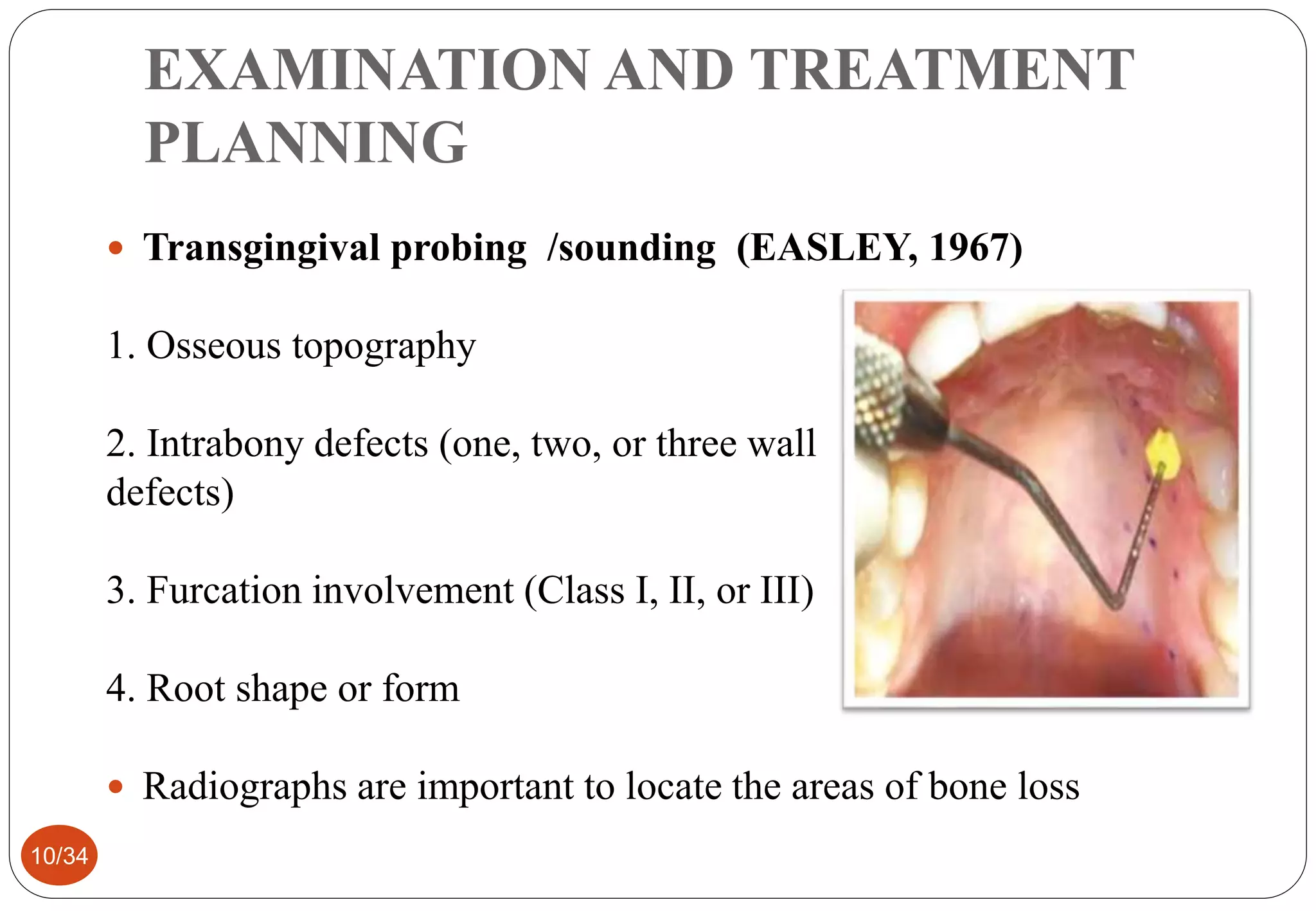
The document provides an overview of resective osseous surgery, detailing its objectives, techniques, and contraindications. It explains the procedures of osteoplasty and ostectomy, which aim to reshape alveolar bone and improve periodontal health. It also reviews the advantages and disadvantages of such surgical interventions, emphasizing their complexity and the necessity for careful treatment planning.