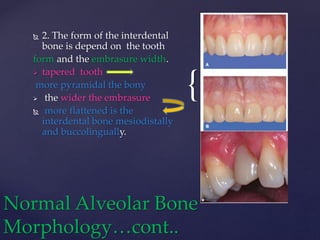
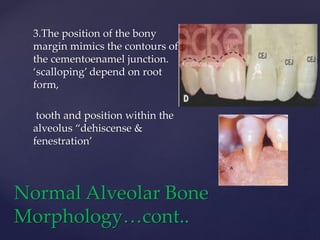
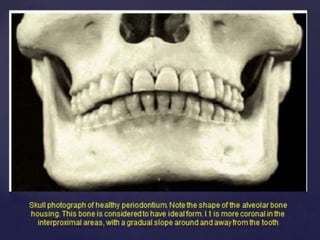
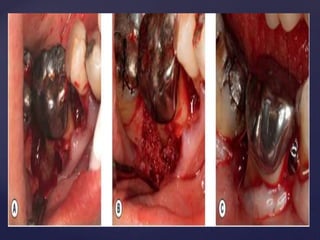
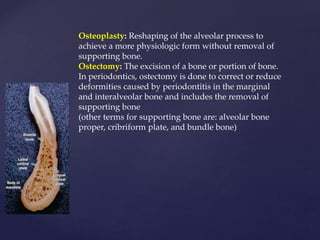
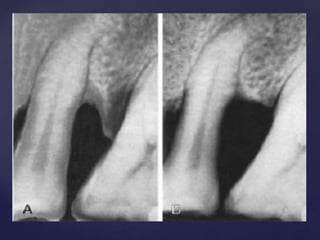
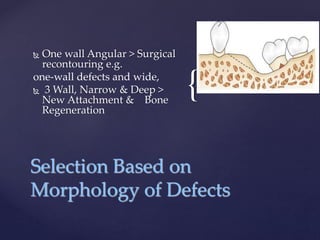
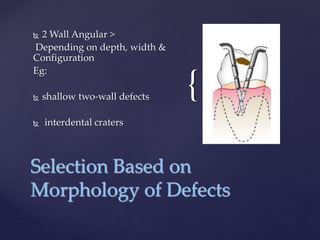
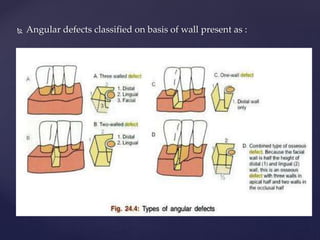
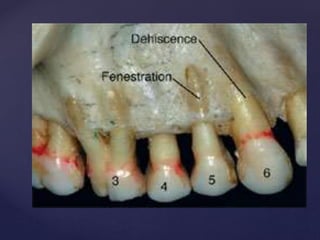
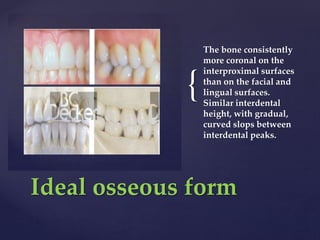
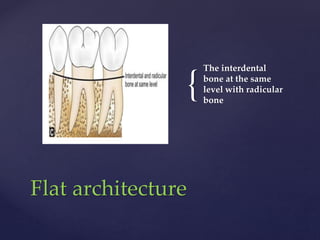
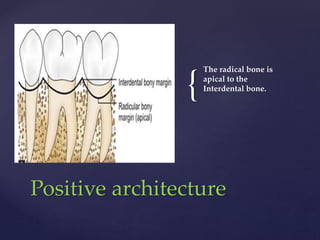
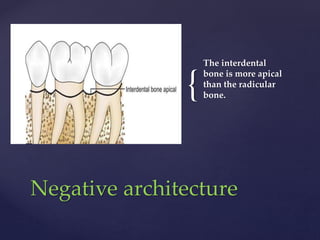
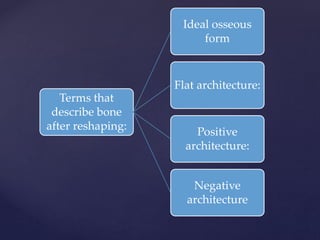
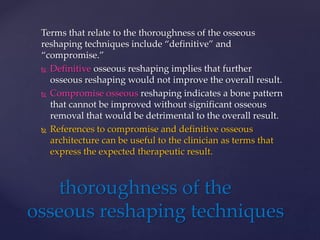
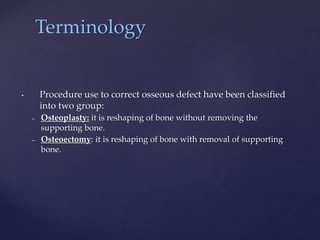
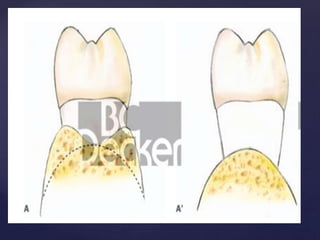
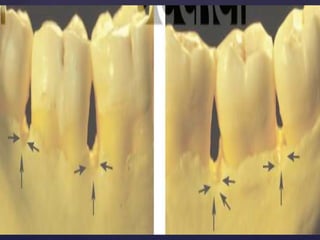
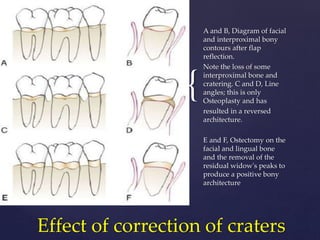
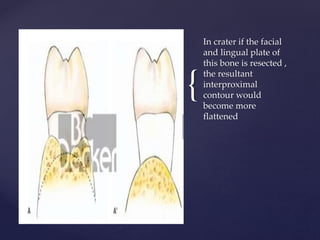
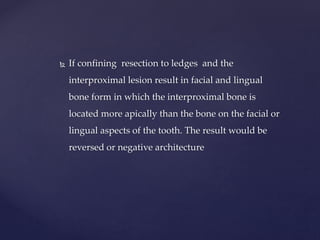
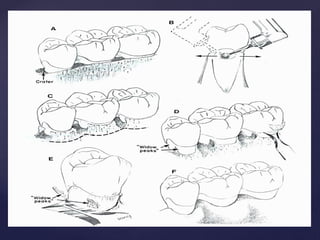
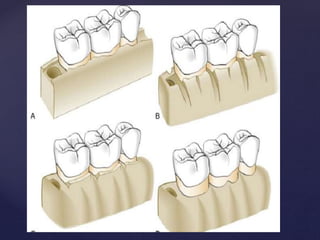
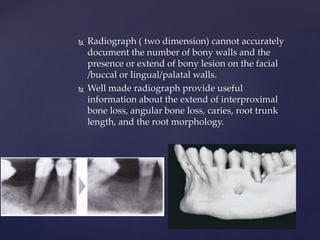
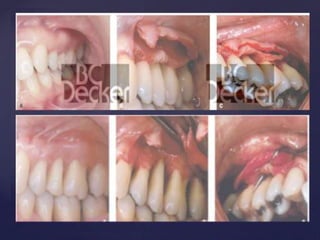
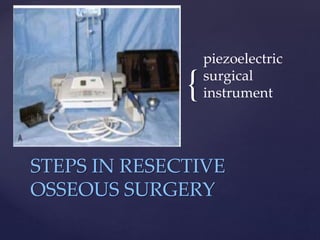
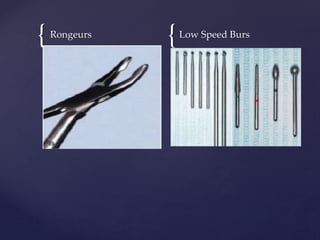
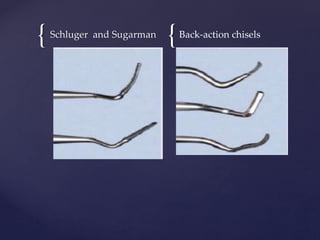
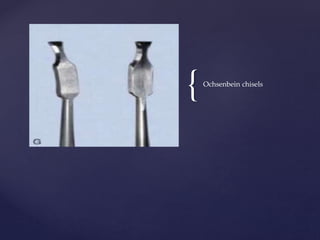
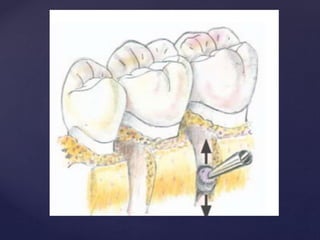
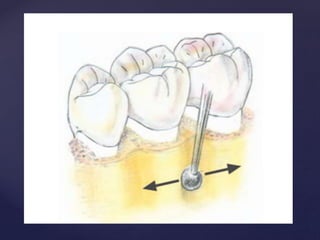
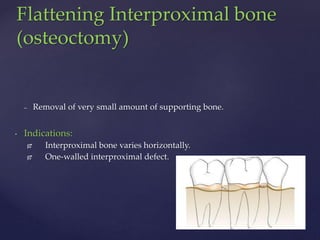
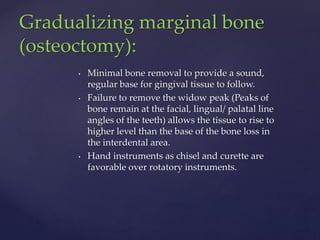
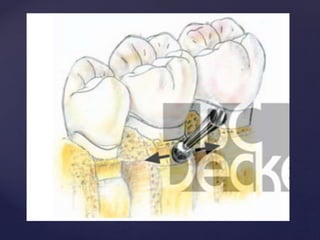
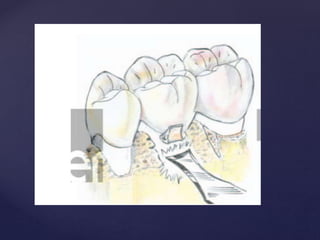
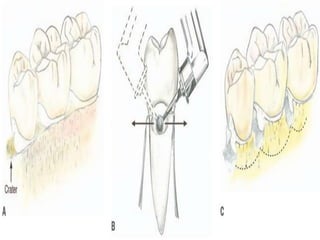
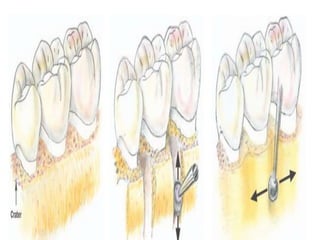
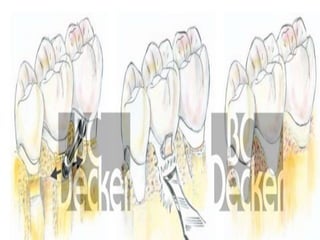
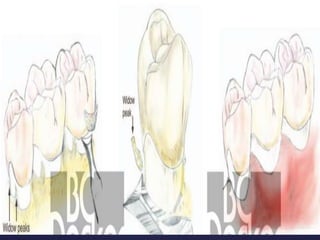
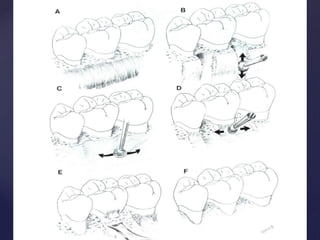
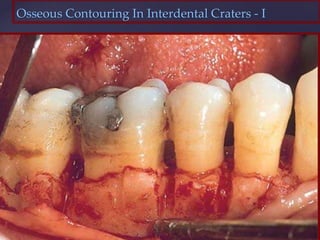
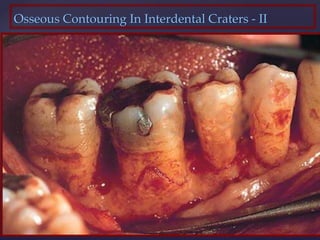
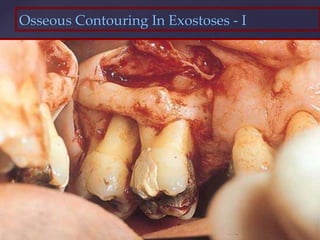
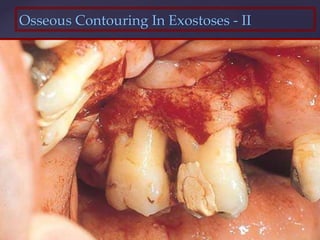
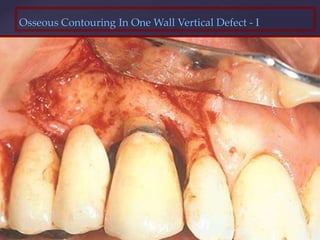
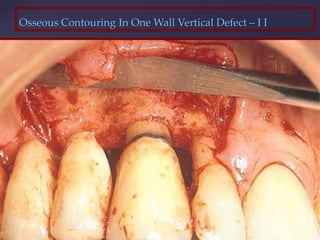
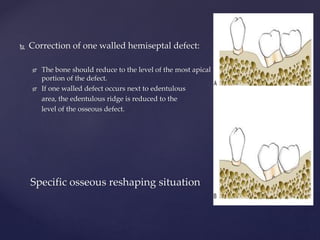
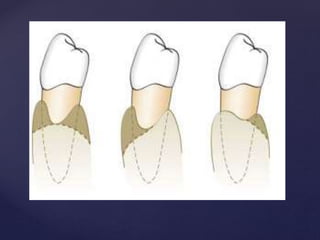
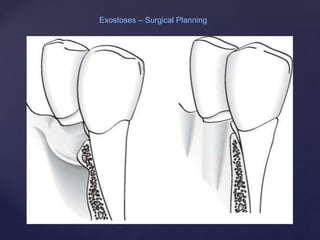
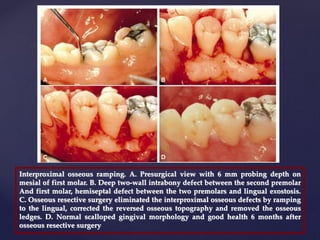
The document discusses principles of resective osseous surgery in periodontal therapy. It outlines the goals of reshaping alveolar bone to eliminate deformities caused by periodontal disease. This involves techniques like osteoplasty to reshape bone without removal and osteotomy to remove supporting bone. Specific procedures are described to correct issues like interdental craters, exostoses, and one-wall defects through techniques like vertical grooving, flattening interproximal bone, and gradualizing marginal bone. Factors in selecting patients and sites for resective surgery and postoperative care are also covered.