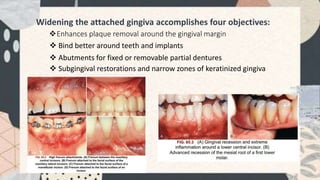
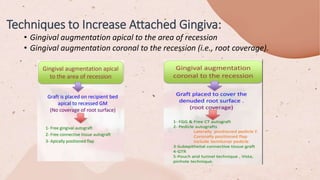
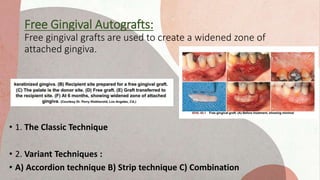
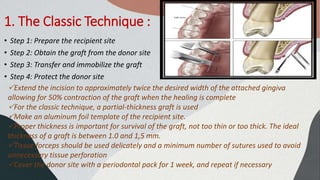
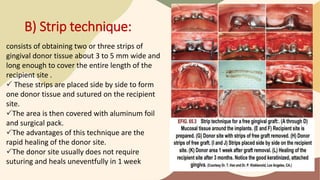
This document discusses the history and techniques of free gingival grafts (FGG), a periodontal plastic surgery procedure used to widen attached gingiva. It describes the classic FGG technique which involves preparing the recipient site, obtaining a partial-thickness graft from the palate donor site, suturing the graft into place, and protecting the donor site. Variant techniques like the accordion, strip, and combination methods are also outlined. The healing process of FGG grafts is explained, noting revascularization begins after 2-3 days and integration is largely complete by 10-17 days, though thicker grafts may take longer. FGG procedures aim to enhance plaque removal, improve tooth stability, and provide tissue