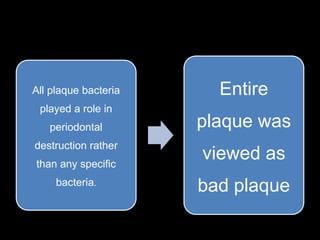
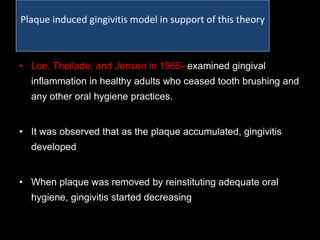
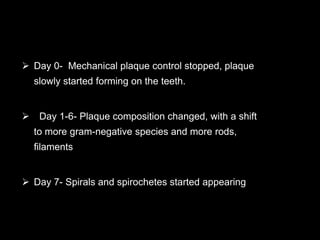
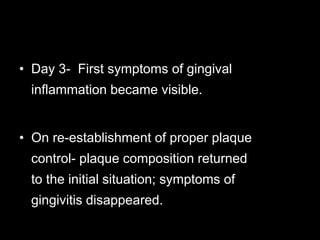
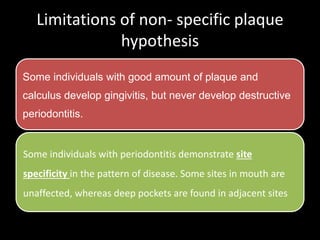
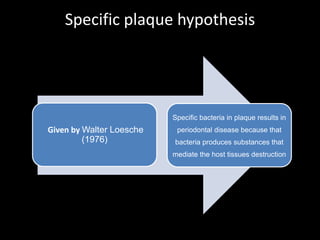
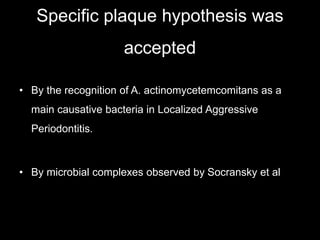
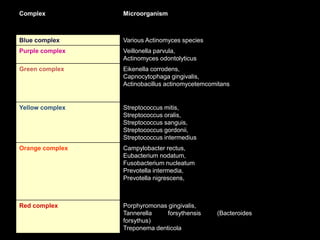
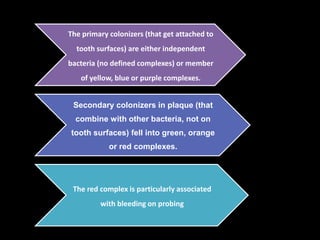
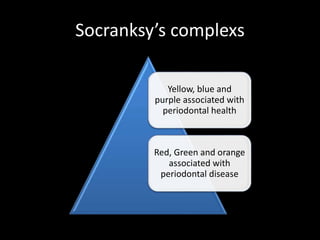
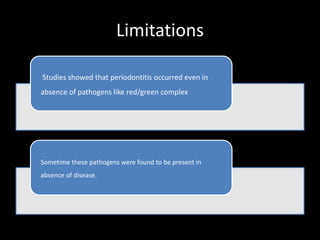
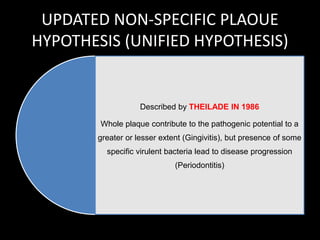
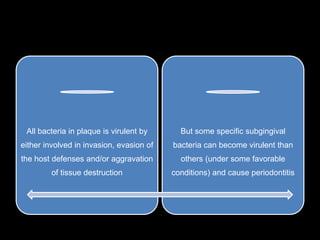
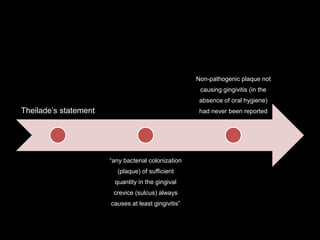
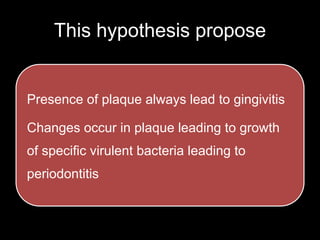
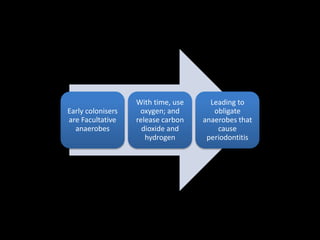
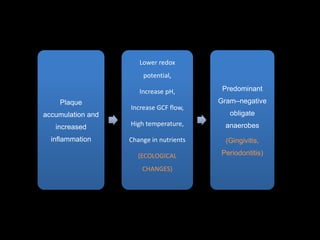
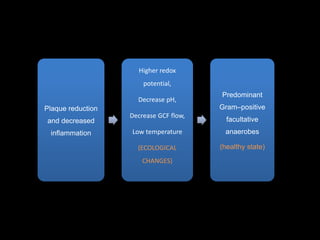
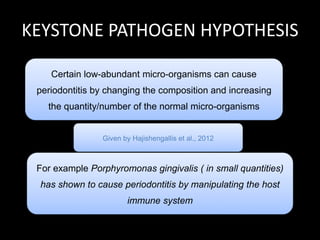
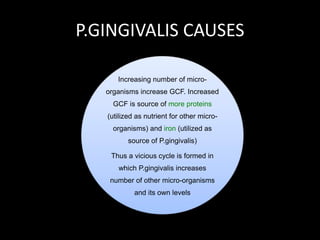
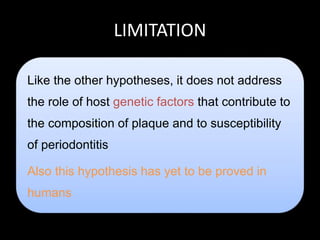
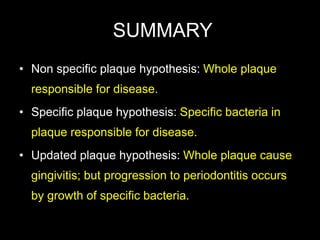
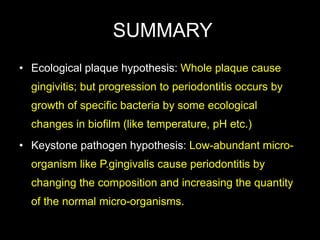
The document discusses various hypotheses regarding the role of plaque in periodontal diseases, including the non-specific, specific, updated, ecological, and keystone pathogen hypotheses. It highlights that while all hypotheses acknowledge plaque accumulation leads to gingivitis, the transition to periodontitis remains complex and not fully explained. A new hypothesis is needed to clarify the intricate interactions between oral microbes and host responses that influence disease progression.