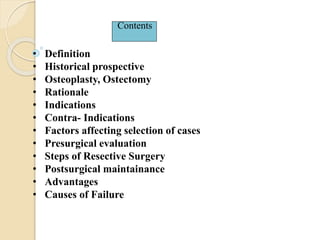
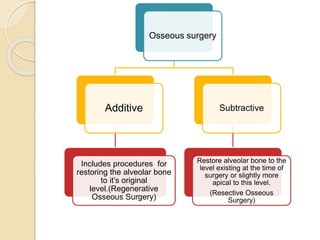
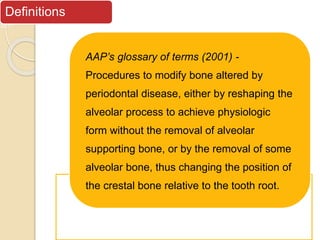
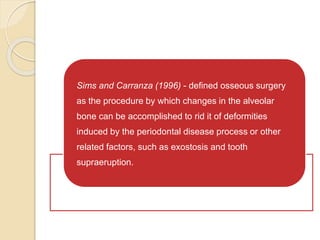
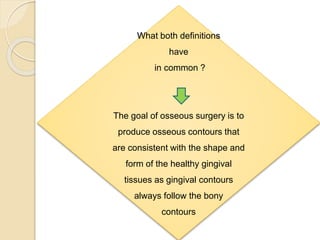
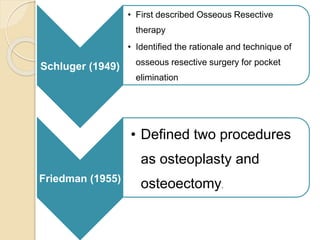
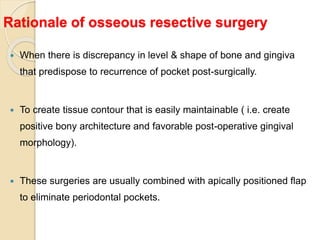
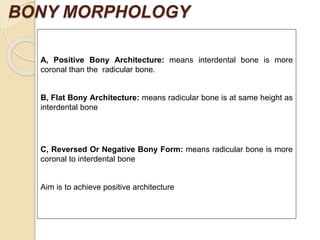
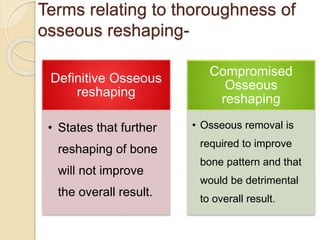
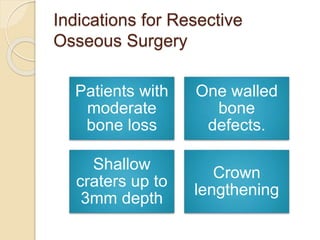
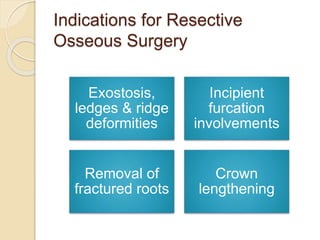
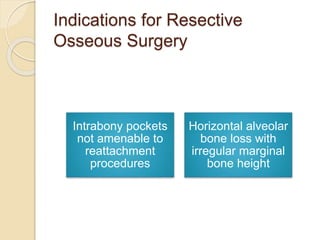
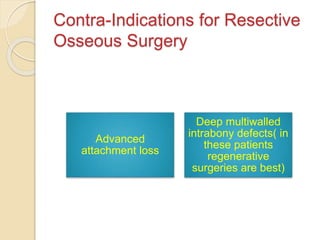
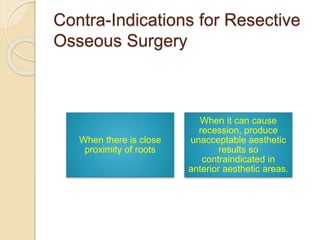
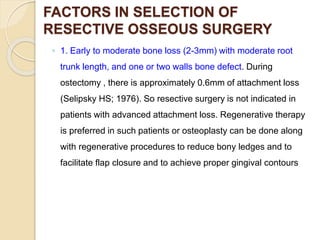
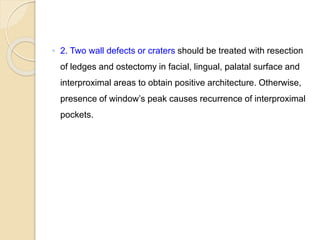
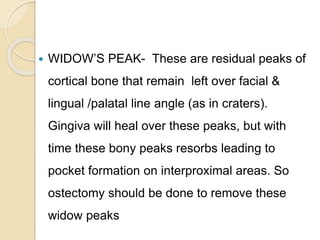
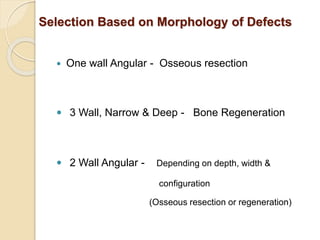
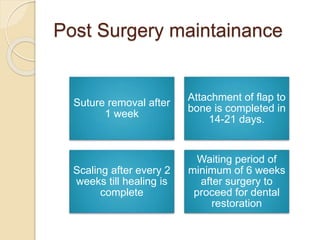
Resective osseous surgery aims to modify and eliminate bony deformities caused by periodontal disease, either through reshaping or removing alveolar bone. Indications for this surgery include moderate bone loss, one-walled defects, and removal of bone abnormalities, with contraindications such as advanced attachment loss and aesthetic concerns. The process involves pre-surgical evaluation, specific surgical techniques to achieve positive bony architecture, and post-surgical maintenance to ensure effective healing and prevent complications.