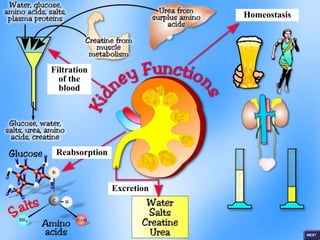
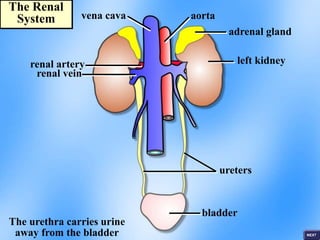
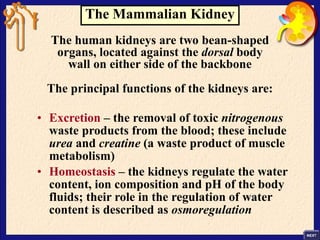
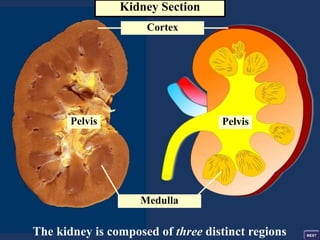
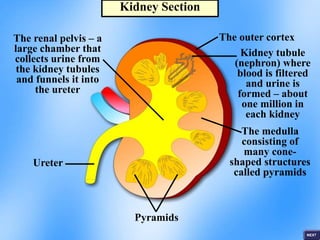
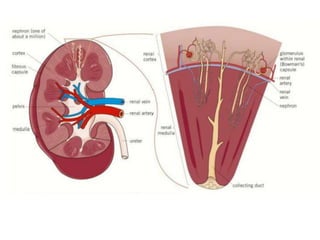
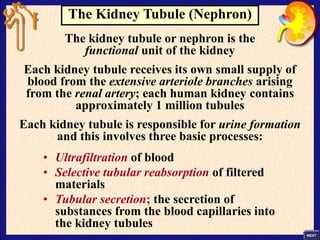
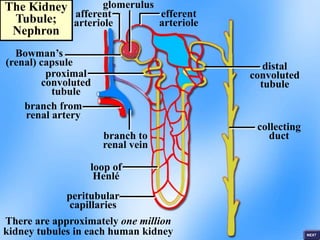
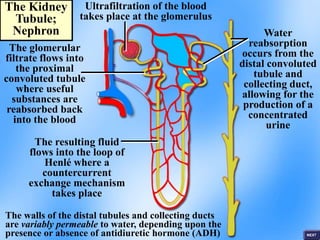
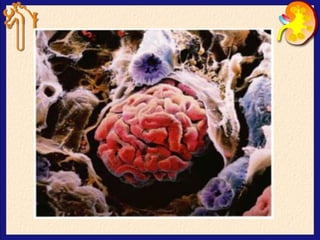
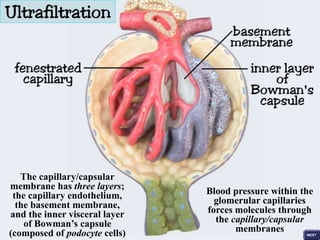
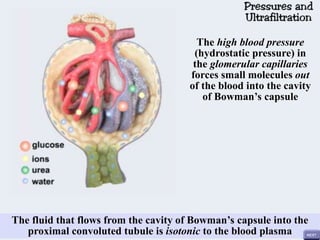
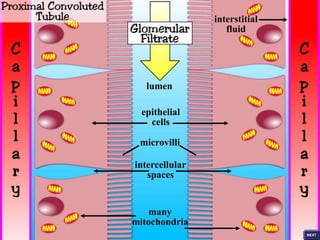
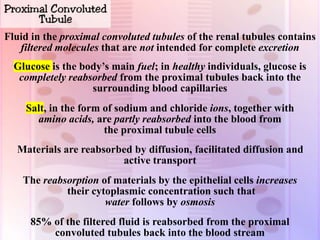
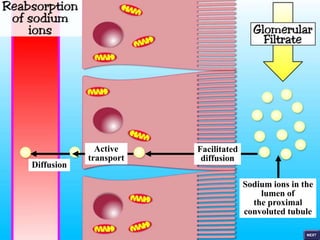
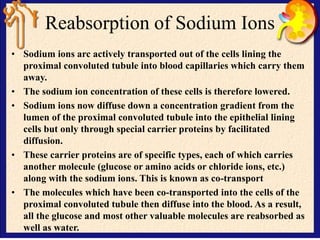
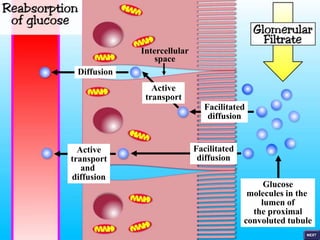
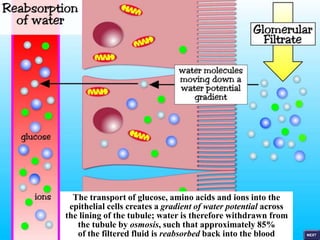
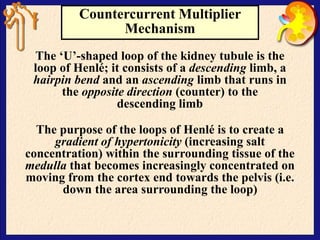
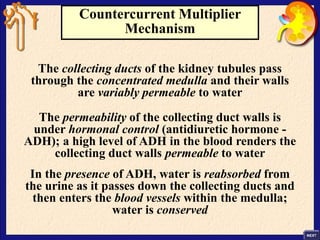
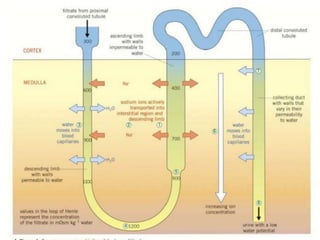
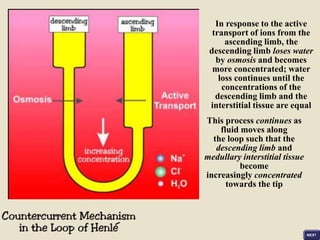
The renal system functions to filter waste from the blood and regulate fluid balance. It contains two kidneys each composed of an outer cortex and inner medulla. The functional unit is the nephron, which filters blood in the glomerulus and reabsorbs nutrients in the proximal tubule. As fluid moves through the loop of Henlé and collecting duct, the countercurrent multiplier mechanism and ADH hormone regulate water reabsorption to produce a concentrated urine.