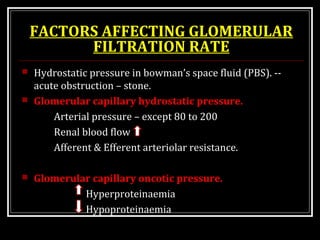
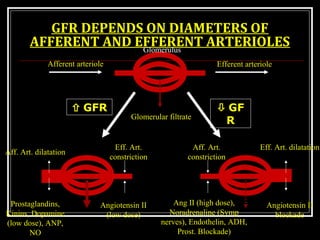
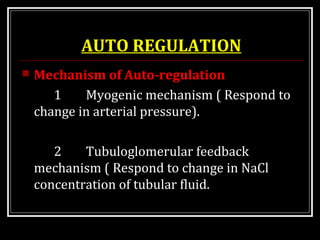
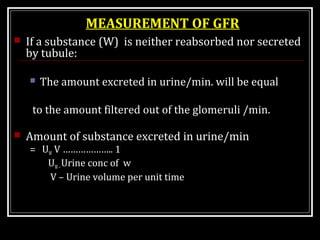
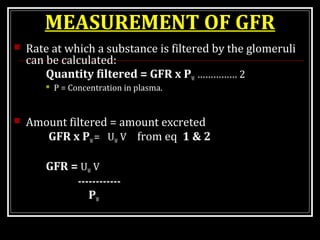
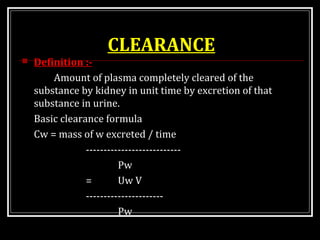
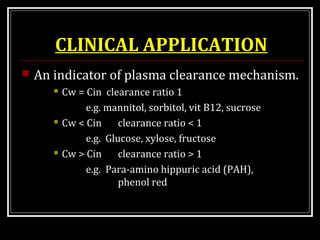
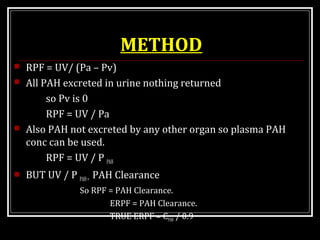
This document provides an overview of urine formation and glomerular filtration rate. It discusses the key parts of nephron involved including glomerulus, Bowman's capsule and different segments of nephron. The three main steps in urine formation are glomerular filtration, tubular reabsorption and tubular secretion. Glomerular filtration is the process by which plasma is filtered into Bowman's space to form primary urine. The rate of glomerular filtration is regulated by various factors like hydrostatic and oncotic pressures in the glomerular capillaries. Glomerular filtration rate can be measured by using clearance of substances like inulin, creatinine and urea that are freely filtered but neither re











![DYNAMICS OF GLOMERULAR
FILTRATION
GFR = KF [(pGc † ΠBS)-(ΠGc † pBS)]](https://image.slidesharecdn.com/urineformation-160601155205/85/URINE-FORMATION-17-320.jpg)
![EFFECTIVE FILTRATION
PRESSURE ( EFP)
EFP=
[(pGc † ΠBS)-(ΠGc † pBS)]
GFR= KF × EFP
= 12.5 [(60 + 0) – (32+18)]
= 12.5 × 10
= 125 ml/min](https://image.slidesharecdn.com/urineformation-160601155205/85/URINE-FORMATION-18-320.jpg)
![FILTRATION
Analysis of Glomerular Capillary Dynamics
GFR = KF [(pGc – pBS)-(ΠGc- ΠBS)]
KF -- filtration coeffiecient = 12.5
pGc - Hydrostatic Pressure Of Glomerular
Capillary = 60.0 mm Hg
pBS – Hydrostatic pressure of bowmans space =
18 mm Hg
ΠGc -oncotic pressure of glomerular cappilary =
32 mm Hg
ΠBS - Oncotic pressure of Bowmans space = 0 mm Hg](https://image.slidesharecdn.com/urineformation-160601155205/85/URINE-FORMATION-19-320.jpg)