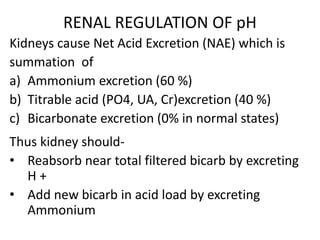
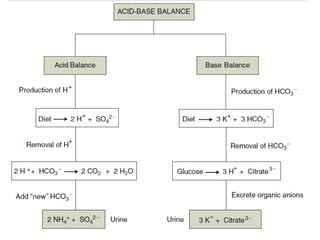
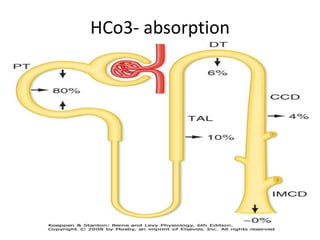
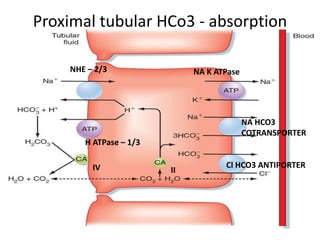
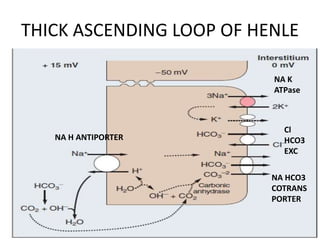
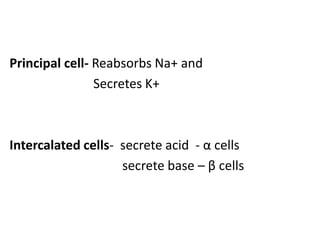
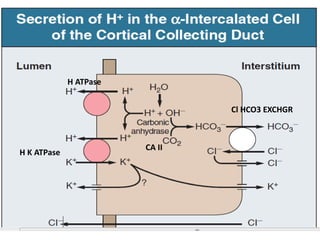
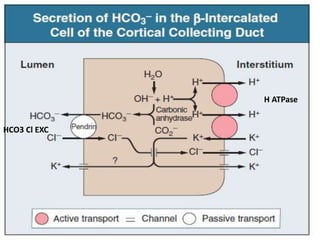
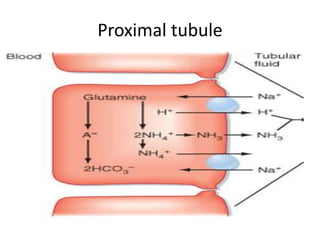
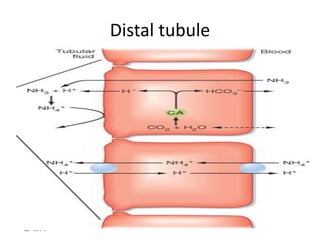
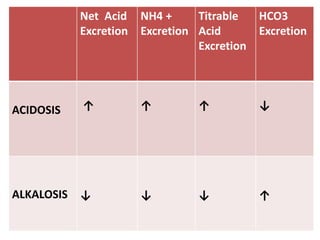
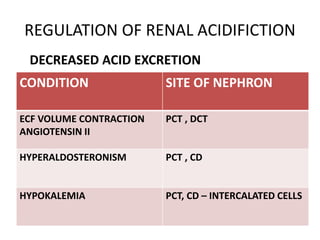
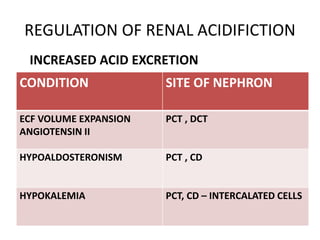
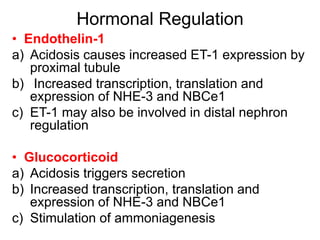
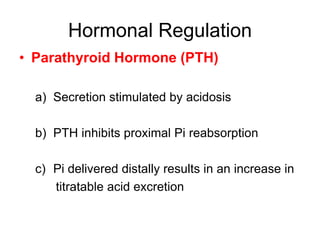
The kidneys play a major role in regulating pH levels in the body through net acid excretion. The kidneys reabsorb nearly all filtered bicarbonate and add new bicarbonate during acid loads by excreting ammonium. Proximal tubular absorption of bicarbonate occurs through NHE-2, NHE-3, and H+-ATPase transporters. Distal tubular acidification involves reabsorption of remaining bicarbonate and secretion of fixed acids and ammonium through buffering and recycling in the collecting duct. Hormones like endothelin-1, glucocorticoids, and PTH regulate renal acidification in response to acid-base conditions.