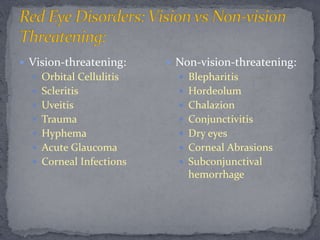
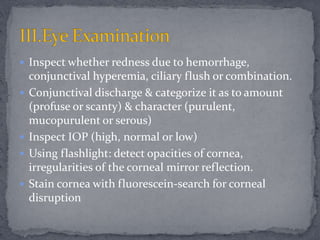
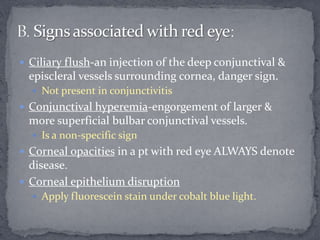
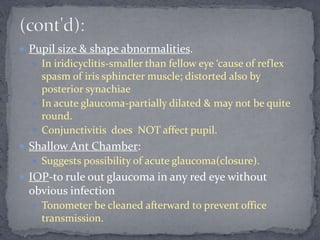
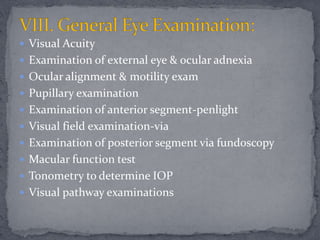
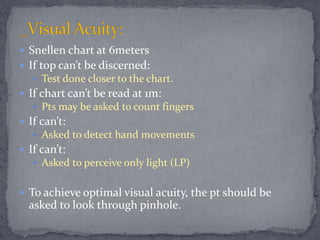
The document provides guidance on evaluating patients presenting with red eye, noting that it can be caused by various ocular diseases ranging from minor irritations to serious conditions. Red eye symptoms and signs are described that can help determine if the cause is vision-threatening, such as blurred vision and pain, or non-vision threatening, like itching. Examination of the eye is also outlined to assess factors like conjunctival discharge, corneal opacity, pupil size and shape, and intraocular pressure to identify potential conditions causing the red eye.