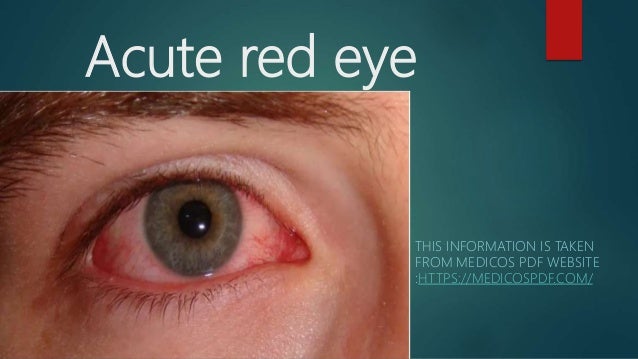
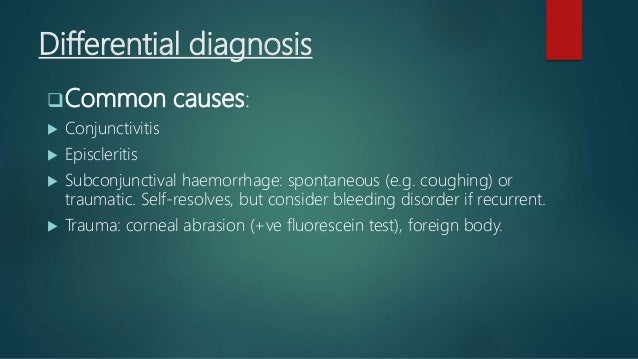
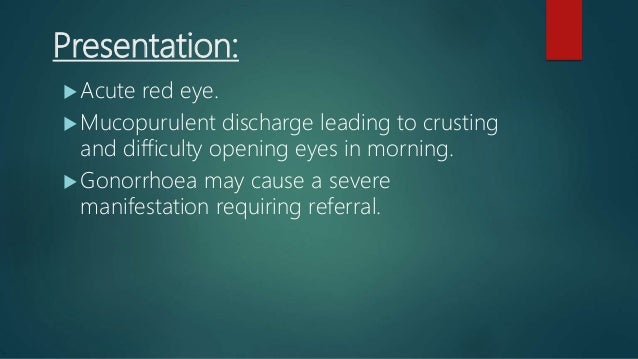
The document discusses various causes and management of acute red eye conditions, including conjunctivitis, episcleritis, scleritis, and others, emphasizing their presentations and treatments. Common causes are detailed alongside their symptoms and recommended interventions such as topical lubricants, antibiotics, and urgent referrals for severe cases. It highlights the importance of proper eye care and management to prevent complications and preserve vision.