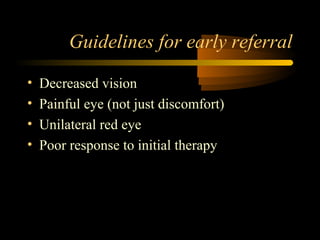
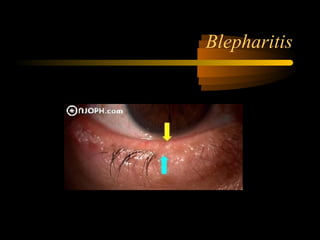
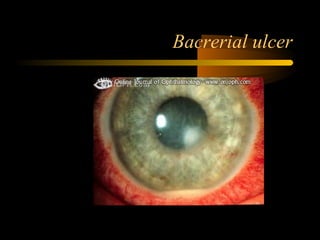
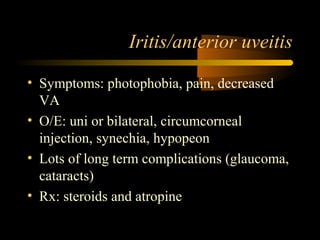
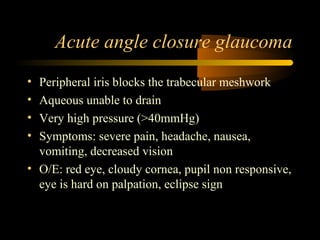
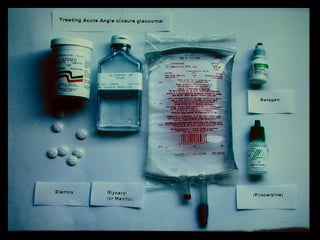
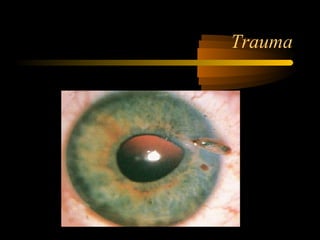
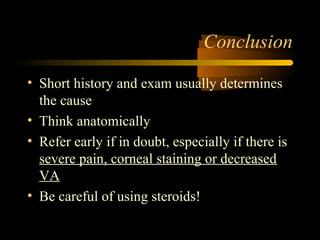
This document provides an overview of common causes of a red eye and guidelines for evaluation and management. It discusses various conditions that can affect the eyelids, conjunctiva, sclera, cornea, iris and anterior chamber. Conditions range from self-limiting issues like blepharitis, styes and viral conjunctivitis to more serious conditions like bacterial ulcers, iritis, uveitis and acute angle closure glaucoma which require prompt referral. A basic history of symptoms and external exam can help form a differential diagnosis, while fluorescein staining aids examination of the cornea. Early referral is advised for decreased vision, severe pain, poor response to initial treatment or unilateral red eye.