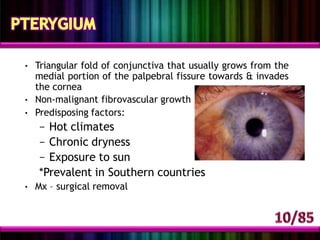
Red eye, or ocular hyperemia, is caused by enlarged, dilated blood vessels leading to redness of the eye's surface. It can be caused by various conditions affecting the conjunctiva, cornea, iris, anterior chamber, eyelids, or orbit. Common causes include conjunctivitis (bacterial, viral, allergic), corneal abrasions, iritis, acute glaucoma, eyelid disorders like entropion or ectropion, and orbital cellulitis. A thorough history and examination is needed to determine the underlying cause and guide appropriate treatment.