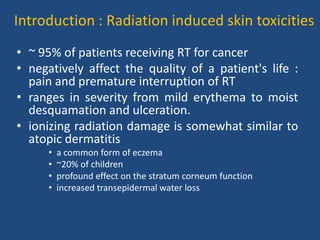
This document discusses the effects of ionizing radiation on skin, including both acute and late effects. It notes that radiation can cause a range of skin reactions from mild erythema to moist desquamation and ulceration. The degree of injury depends on factors like total radiation dose and time interval. Acute effects involve cellular and inflammatory changes in the epidermis and dermis over hours to weeks. Late effects like fibrosis, telangiectasias, and delayed wound healing can occur months to years later. Risk factors include age, gender, and technical factors like radiation dose and site. Several scoring systems are presented to grade skin reactions. Treatment focuses on wound care, topical agents, antibiotics and growth factors to promote healing