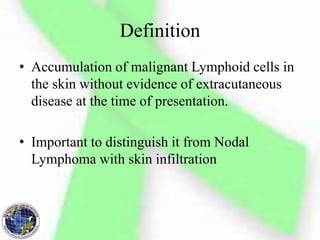
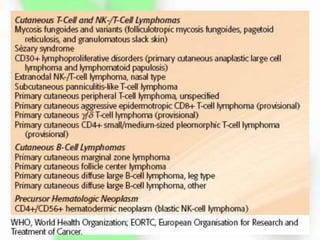
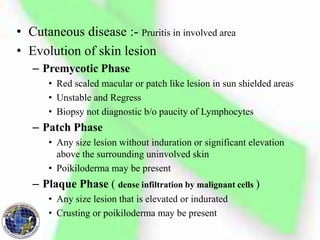
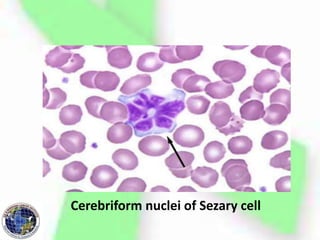
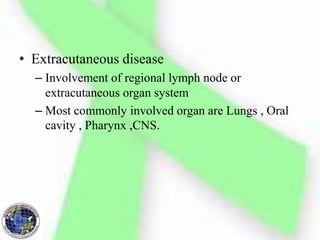
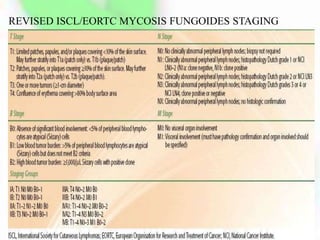
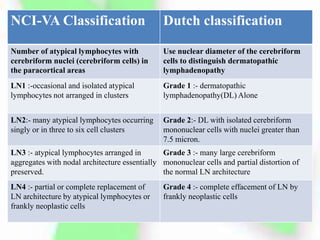
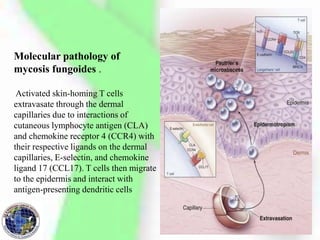
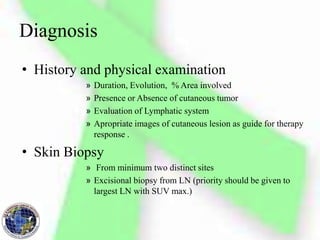
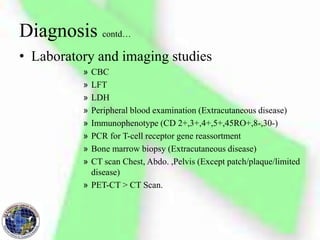
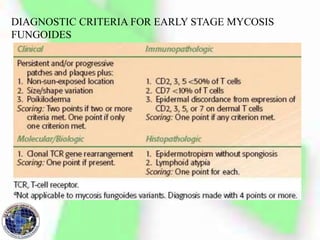
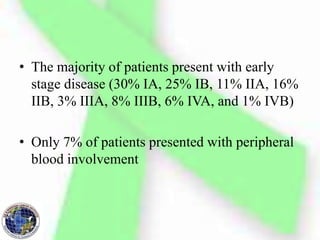
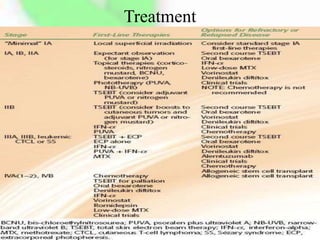
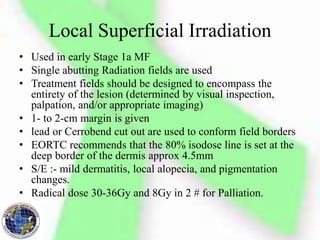
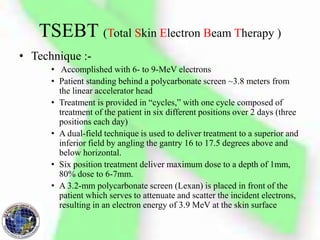
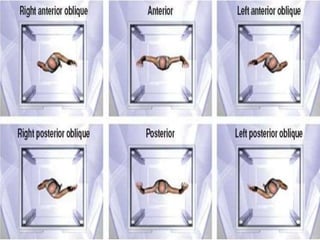
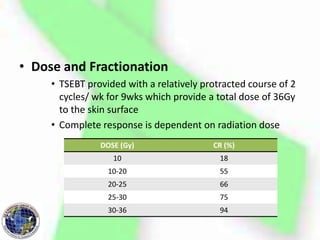
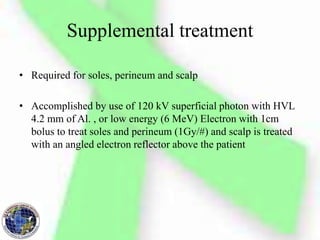
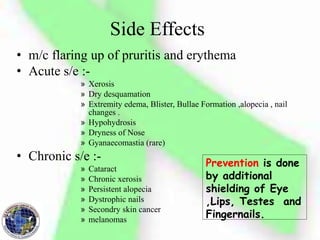
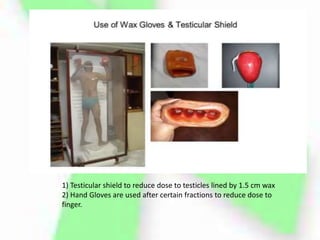
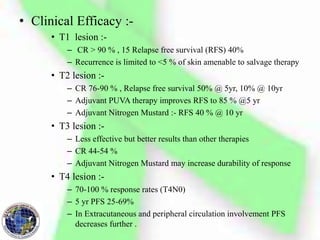
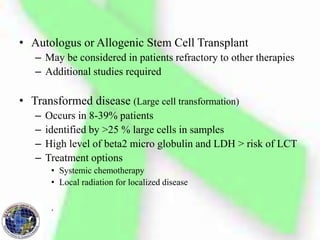
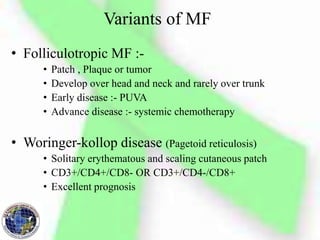
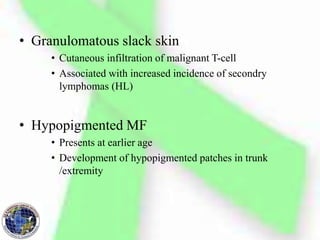
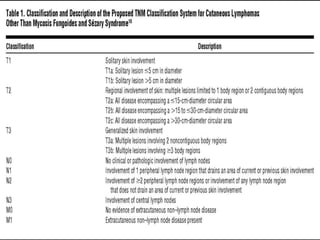
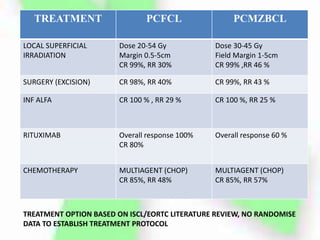
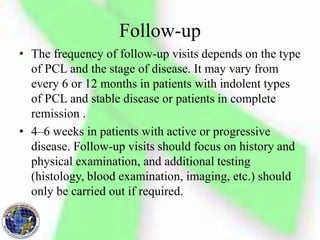
Primary cutaneous lymphoma is a type of non-Hodgkin lymphoma that presents in the skin without evidence of extracutaneous disease. Mycosis fungoides is the most common type of cutaneous T-cell lymphoma, presenting as patches and plaques on the skin that can progress to tumors. Treatment depends on the stage of disease and includes skin-directed therapies like radiation and phototherapy for early stages and systemic therapies for advanced disease. Prognosis is generally good for early stage mycosis fungoides but worsens with increasing stage and extracutaneous spread.