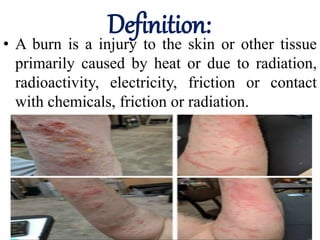
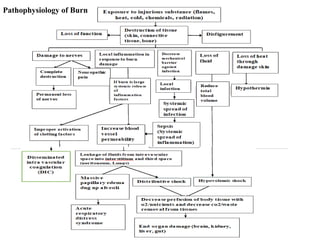
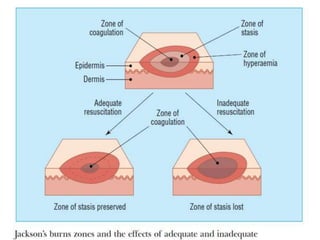
This document provides information on burns, including causes, types, assessment, management, and treatment. It discusses:
- The different causes of burns, including thermal, electrical, chemical, and radiation burns.
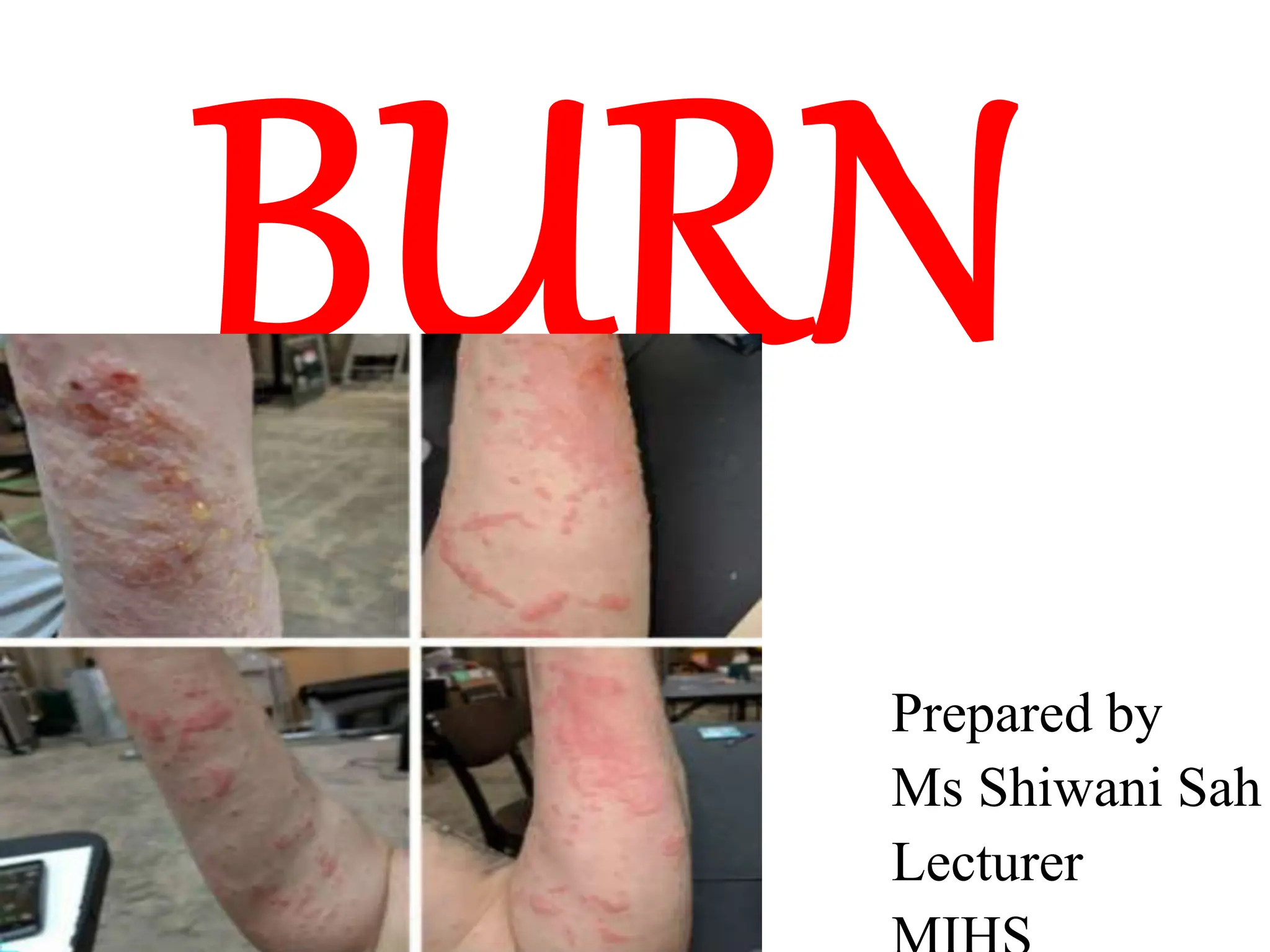
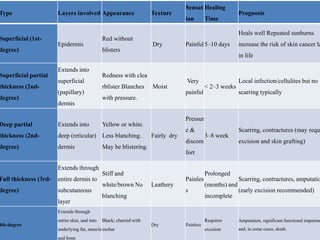
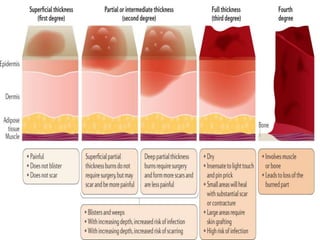
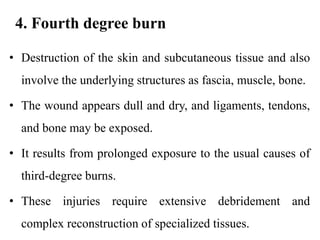
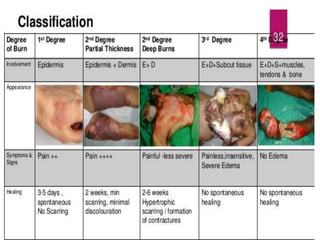
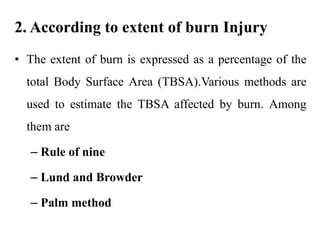
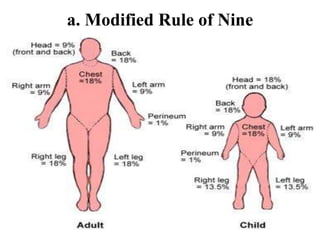
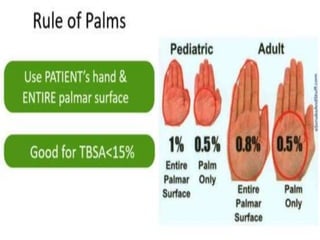
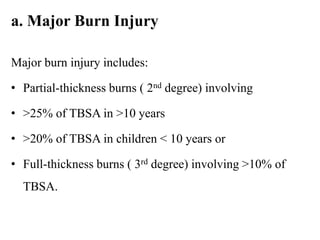
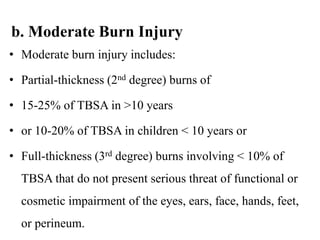
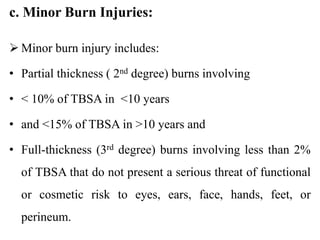
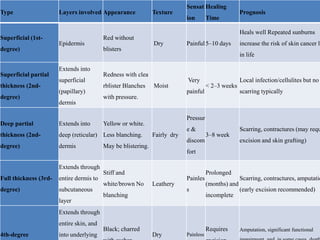
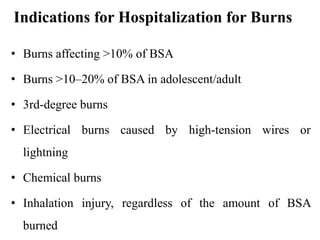
- How to assess burn severity based on depth and extent of damage. Burns are typically classified as superficial, partial thickness, full thickness, or fourth degree.
- The signs and symptoms associated with different burn depths. More severe burns involve deeper tissue damage and have a poorer prognosis.
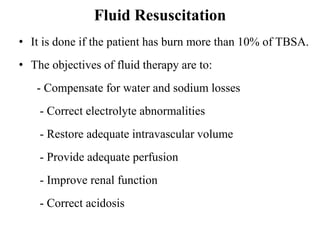
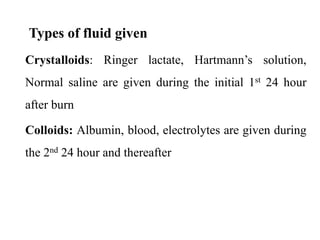
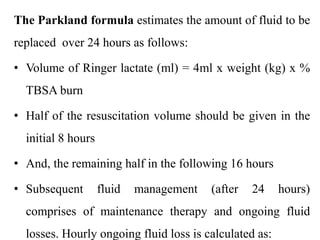
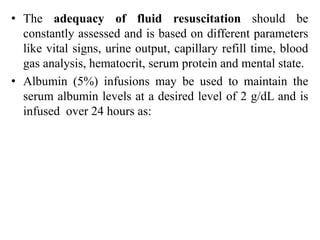
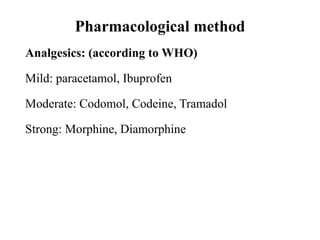
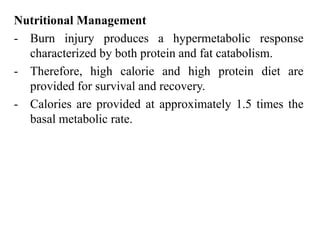
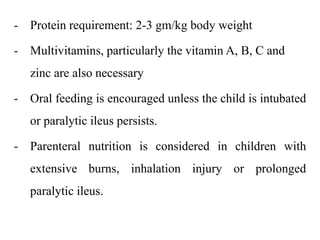
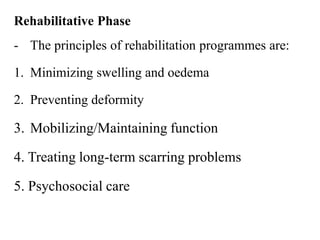
- The three phases of burn management: emergent/resuscitative, intermediate, and rehabilitative. The emergent phase focuses on initial first aid, ABCDE assessment, pain management and fluid resuscitation
![Laboratory and diagnostic tests
• Complete blood count—decreased
• Arterial blood gas values—metabolic acidosis
(decreased pH, increased partial pressure of carbon
dioxide [Pco2], and decreased partial pressure of
oxygen [Po2])
• Serum electrolyte levels—decreased because of loss to
traumatized areas and interstitial spaces
• Serum glucose level—increased because of stress-
invoked glycogen breakdown or glyconeogenesis](https://image.slidesharecdn.com/burn-231222063923-027e6664/85/burn-pptx-46-320.jpg)