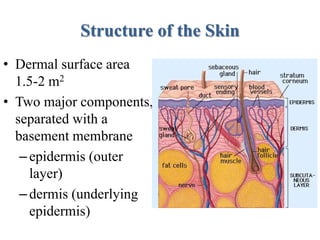
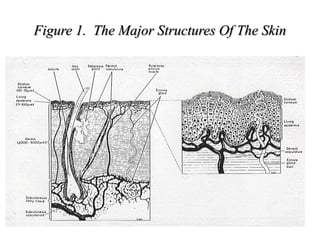
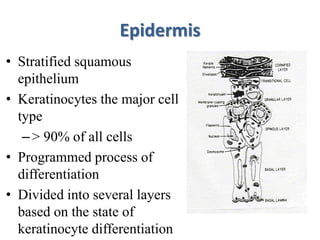
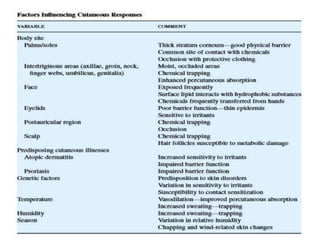
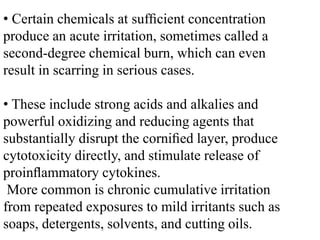
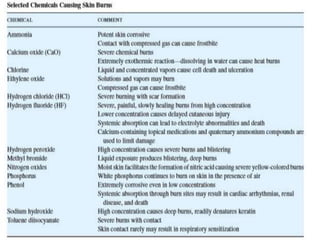
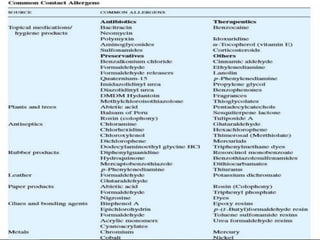
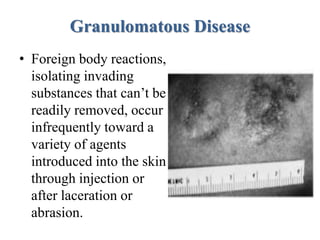
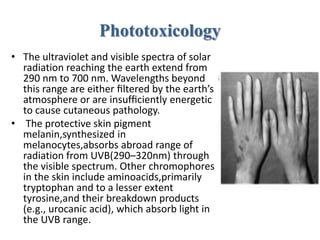
This document summarizes skin toxicology. It discusses the structure and functions of the skin, percutaneous absorption, and various skin diseases and conditions including occupational skin diseases, contact dermatitis, phototoxicity, granulomatous disease, acne, pigmentary disturbances, urticaria, toxic epidermal necrolysis, and skin cancer. It provides details on the causes, mechanisms, and characteristics of these diseases and conditions.