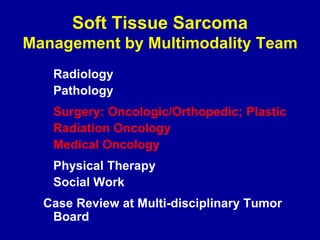
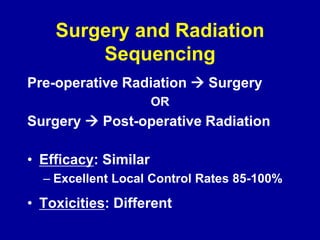
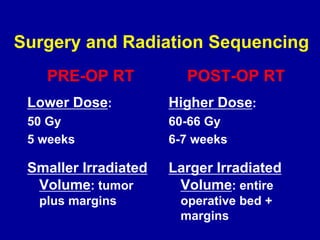
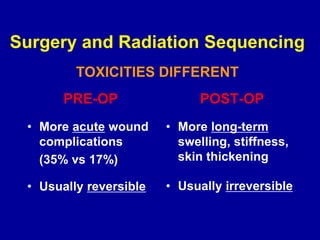
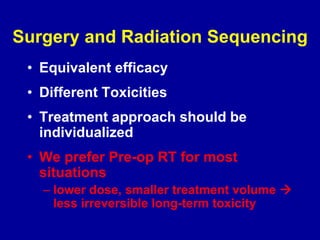
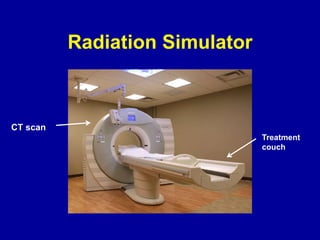
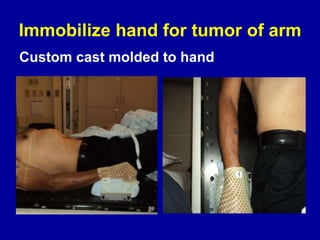
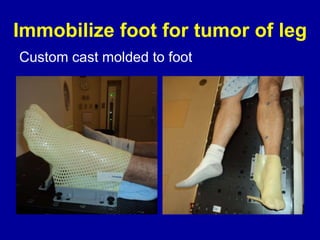
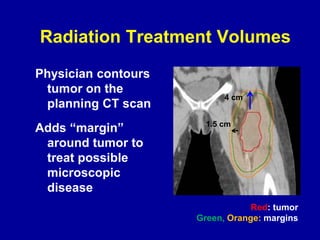
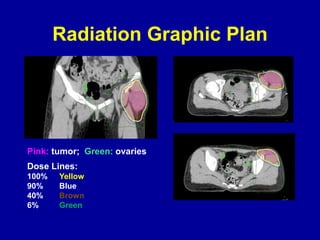
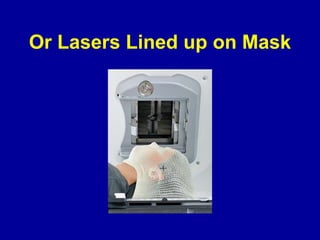
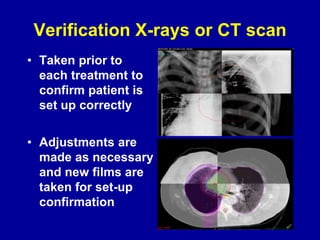
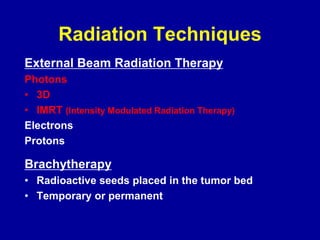
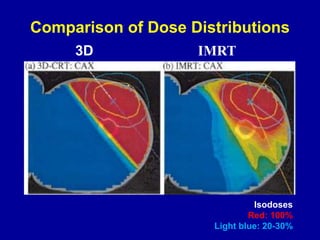
The document discusses the management of soft tissue sarcoma, emphasizing a multimodal approach involving surgery, radiation, and systemic therapy at experienced centers for better outcomes. It compares pre-operative and post-operative radiation sequencing, noting differences in efficacy and toxicities, and highlights the radiation planning process and techniques used for treatment. Side effects, both acute and chronic, are outlined, along with the expert team at the Dana-Farber/Brigham and Women’s Cancer Center.