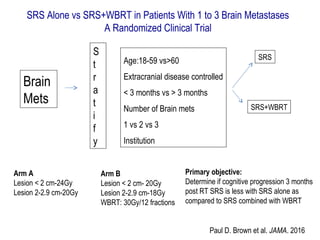
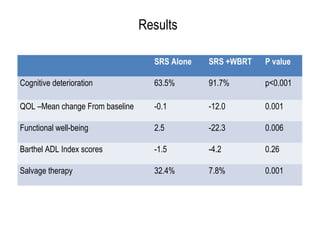
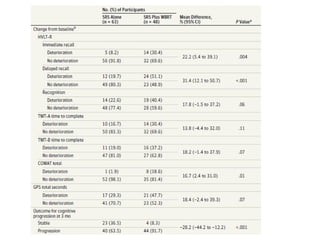
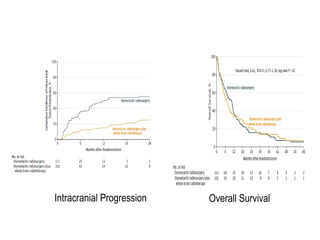
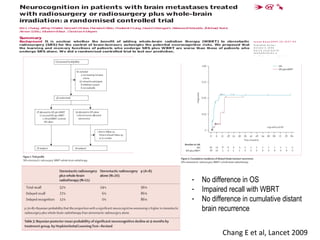
A randomized controlled trial investigated the effects of adding whole-brain radiation therapy (WBRT) to stereotactic radiosurgery (SRS) for patients with newly diagnosed brain metastases. Results indicated that patients receiving SRS alone experienced less cognitive decline compared to those receiving SRS plus WBRT, with a notable difference in learning and memory function after four months. The study supports using SRS as a preferred treatment strategy to better preserve neurocognitive function in these patients.
![Analysis 1.1. Comparison 1 Whole-Brain Radiotherapy versus Observation, Outcome 1 Overall Survival.
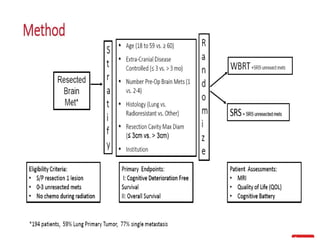
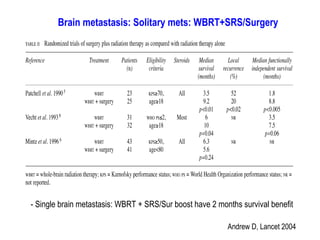
Review: Surgery or radiosurgery plus whole brain radiotherapy versus surgery or radiosurgery alone for brain metastases
Comparison: 1 Whole-Brain Radiotherapy versus Observation
Outcome: 1 Overall Survival
Study or subgroup
Whole-Brain
Radiotherapy Observation log [Hazard Ratio] Hazard Ratio Weight Hazard Ratio
N N (SE) IV,Random,95% CI IV,Random,95% CI
Patchell 1998 49 46 -0.09 (0.22) 21.5 % 0.91 [ 0.59, 1.41 ]
Aoyama 2006 65 67 0 (0.19) 24.6 % 1.00 [ 0.69, 1.45 ]
Roos 2006 10 9 0.01 (0.52) 6.6 % 1.01 [ 0.36, 2.80 ]
Chang 2009 28 30 0.9 (0.31) 14.5 % 2.46 [ 1.34, 4.52 ]
Kocher 2011 180 179 -0.02 (0.12) 32.7 % 0.98 [ 0.77, 1.24 ]
Total (95% CI) 332 331 100.0 % 1.11 [ 0.83, 1.48 ]
Heterogeneity: Tau2 = 0.05; Chi2 = 8.34, df = 4 (P = 0.08); I2 =52%
Test for overall effect: Z = 0.72 (P = 0.47)
Test for subgroup differences: Not applicable
0.5 0.7 1 1.5 2
Favours WBRT Favours Observation
Soon et al, Cochrene metaanalysis, 2014
Brain metastasis: Cochrane meta-analysis 2014
Surgery/SRS+ WBRT Vs SRS/Surgery alone: Over all Survival
No difference in over all survival
p-value=0.47](https://image.slidesharecdn.com/brainmets-170820090429/85/Radiosurgery-in-Brain-Metastases-11-320.jpg)
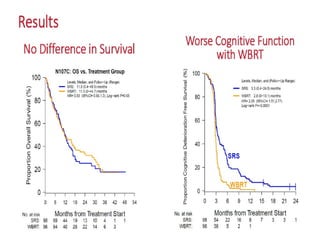
![Analysis 1.2. Comparison 1 Whole-Brain Radiotherapy versus Observation, Outcome 2 Progression Free
Survival.
Review: Surgery or radiosurgery plus whole brain radiotherapy versus surgery or radiosurgery alone for brain metastases
Comparison: 1 Whole-Brain Radiotherapy versus Observation
Outcome: 2 Progression Free Survival
Study or subgroup
Whole-Brain
Radiotherapy Observation log [Hazard Ratio] Hazard Ratio Weight Hazard Ratio
N N (SE) IV,Random,95% CI IV,Random,95% CI
Kocher 2011 180 179 -0.34 (0.11) 88.4 % 0.71 [ 0.57, 0.88 ]
Roos 2006 10 9 0.24 (0.52) 11.6 % 1.27 [ 0.46, 3.52 ]
Total (95% CI) 190 188 100.0 % 0.76 [ 0.53, 1.10 ]
Heterogeneity: Tau2 = 0.03; Chi2 = 1.19, df = 1 (P = 0.28); I2 =16%
Test for overall effect: Z = 1.47 (P = 0.14)
Test for subgroup differences: Not applicable
0.5 0.7 1 1.5 2
Favours WBRT Favours Observation
Soon et al, Cochrene metaanalysis, 2014
Brain metastasis: Cochrane meta-analysis 2014
Surgery/SRS+ WBRT Vs SRS/Surgery alone: Progression free Survival
WBRT: Definite reduction in local failure
p-value=0..14](https://image.slidesharecdn.com/brainmets-170820090429/85/Radiosurgery-in-Brain-Metastases-12-320.jpg)