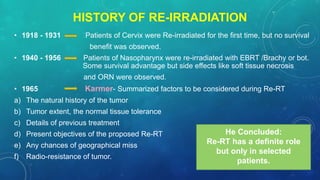
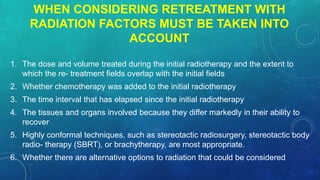
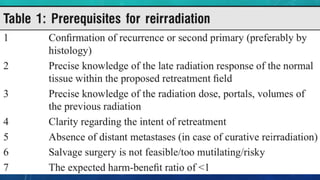
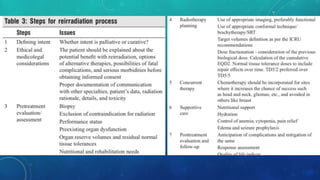
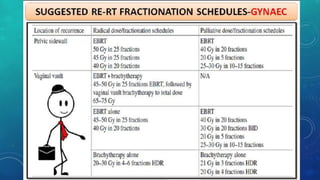
- Reirradiation or retreatments after initial radiotherapy is possible for 10% of cancer patients who experience a second cancer. However, if the radiation tolerance of a normal organ or tissue was exceeded in the initial treatment, reirradiation cannot be done safely.
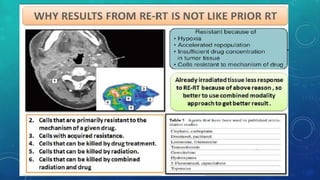
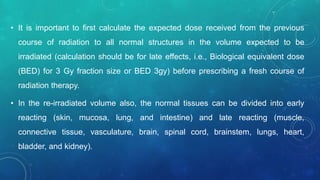
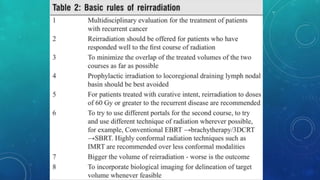
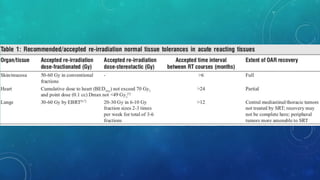
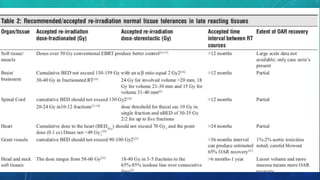
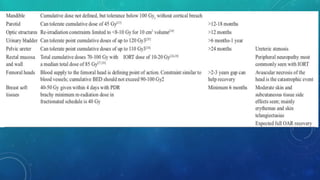
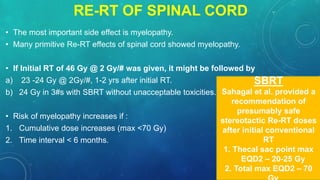
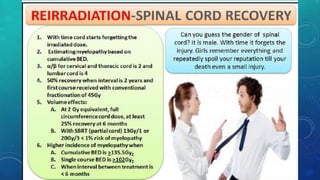
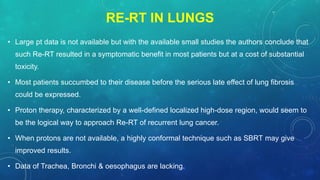
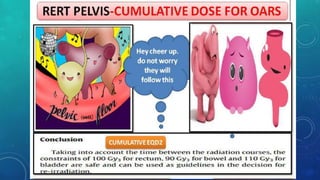
- Early-responding tissues like skin generally recover better than late-responding tissues like fibrosis and can tolerate reirradiation with reduced doses. Spinal cord and lung data from rodent and monkey studies show some reirradiation is possible. Kidney and bladder do not recover from late damage.
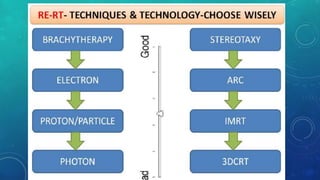
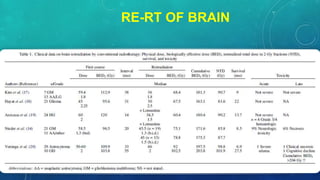
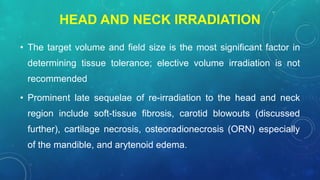
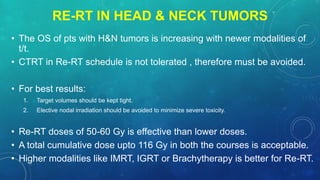
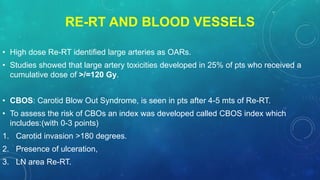
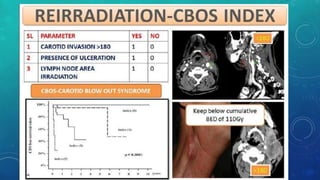
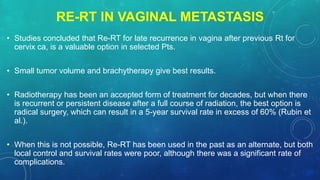
- Clinical studies on reirradiation are limited but show it can provide local control and possibly survival for head and neck cancers, though with high risks of toxicity and functional