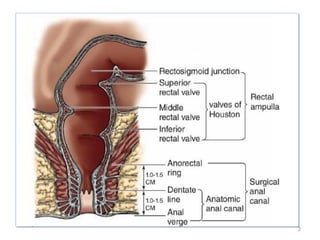
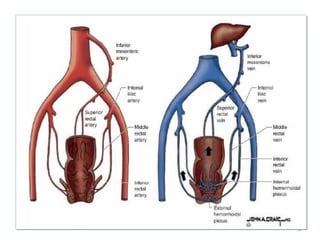
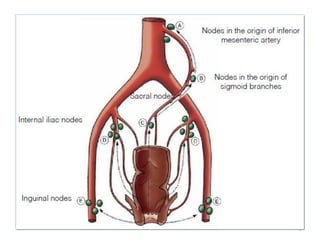
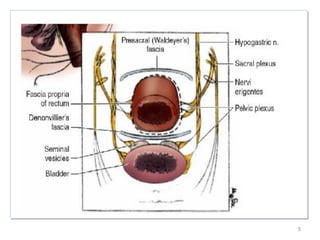
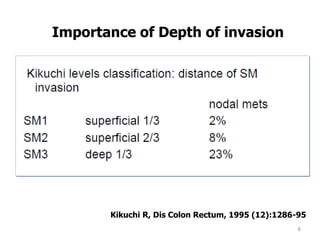
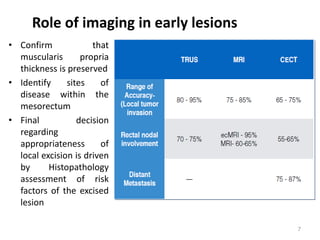
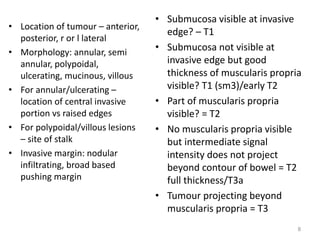
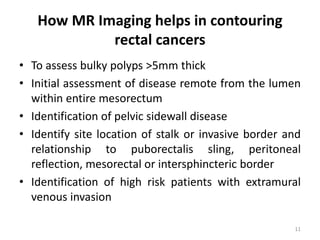
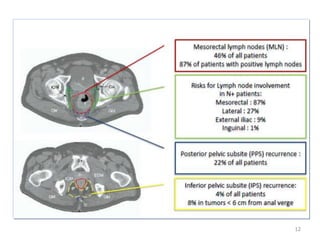
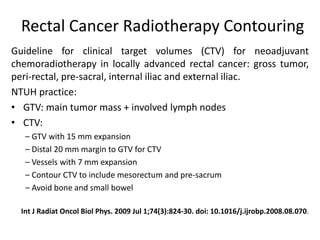
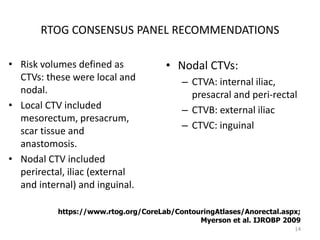
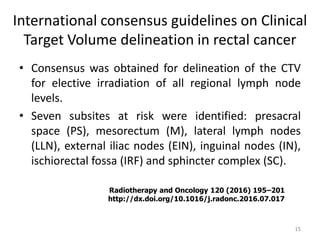
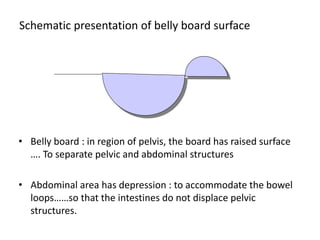
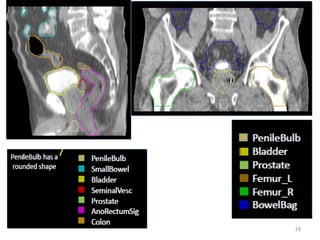
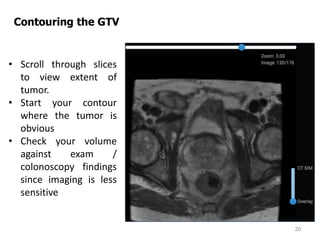
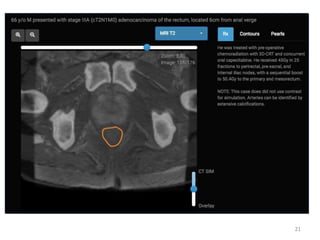
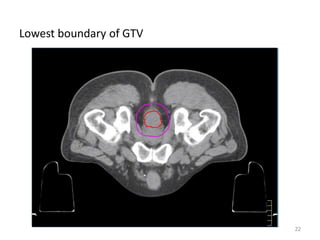
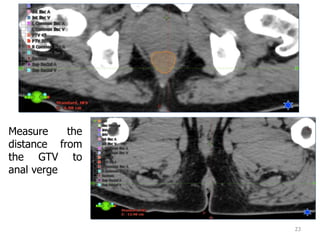
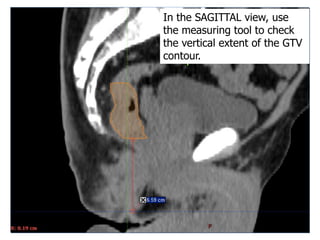
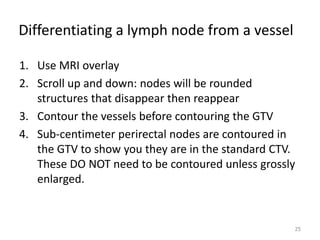
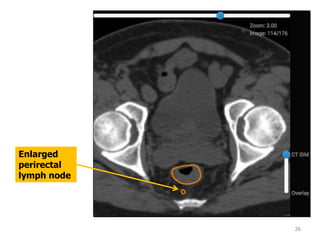
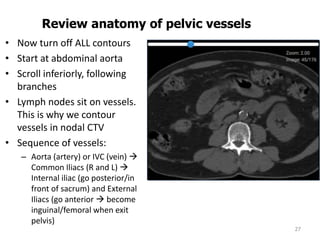
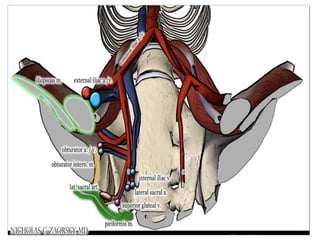
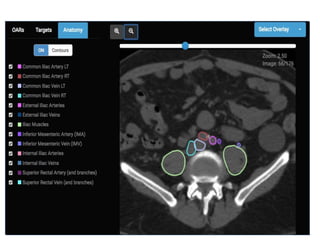
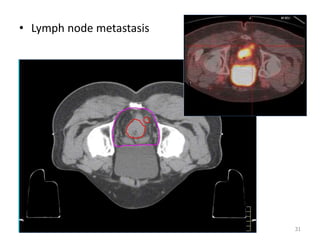
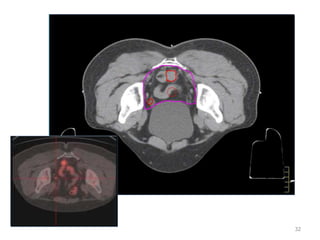
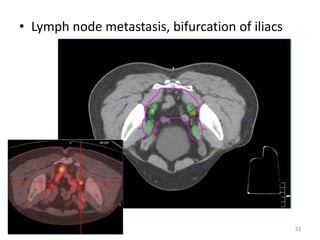
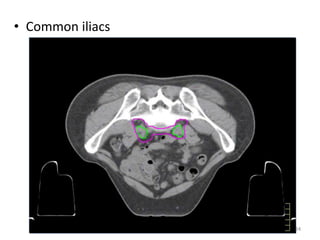
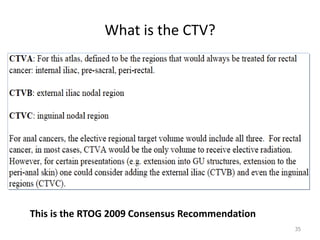
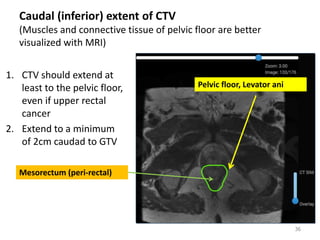
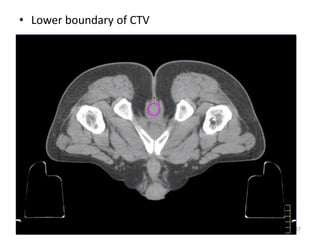
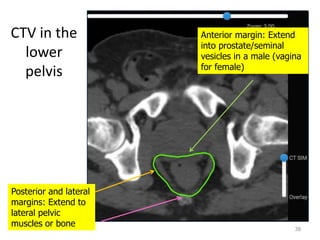
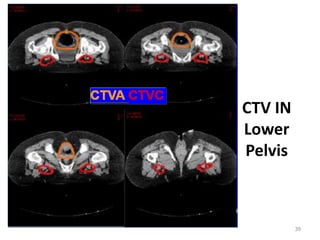
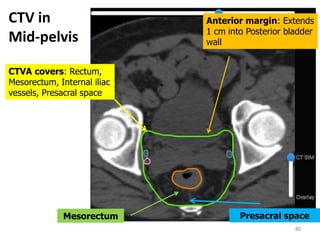
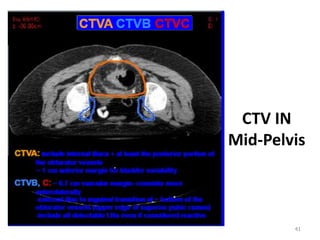
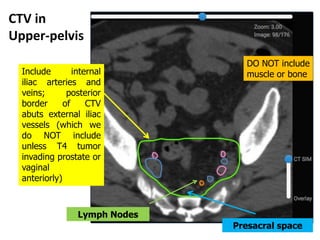
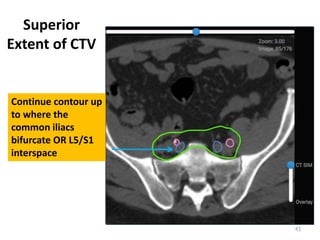
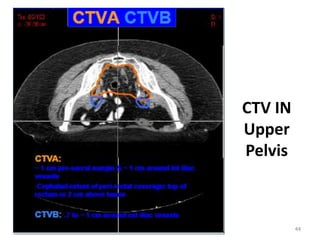
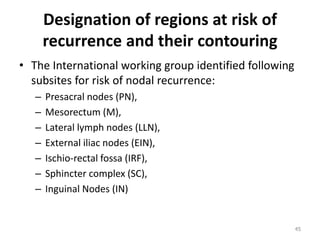
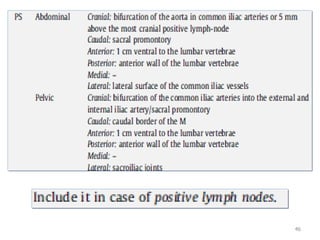
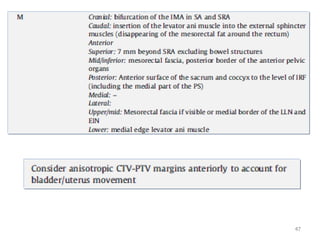
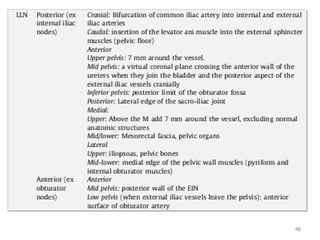
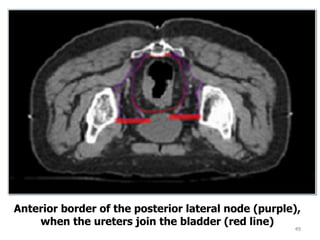
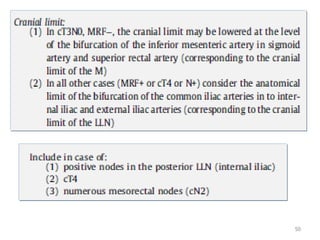
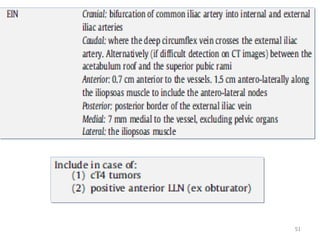
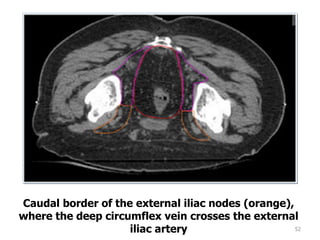
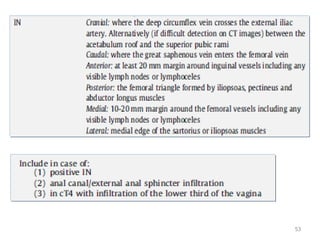
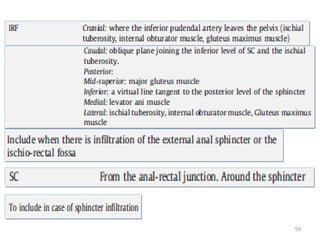
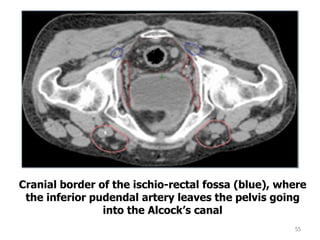
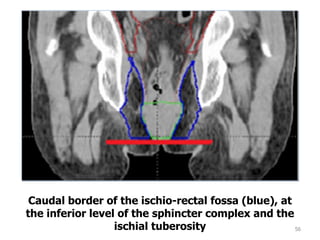
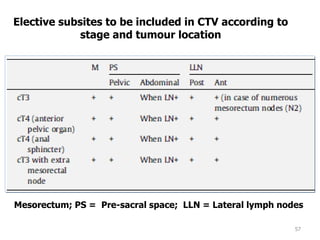
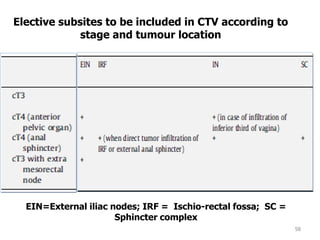
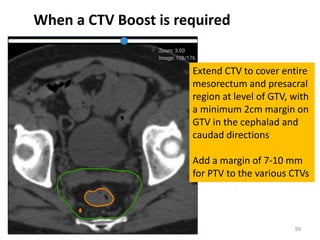
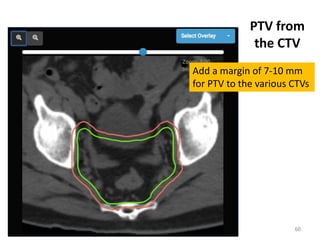
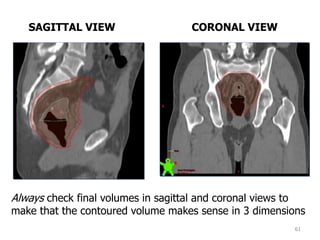
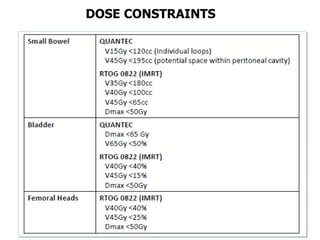
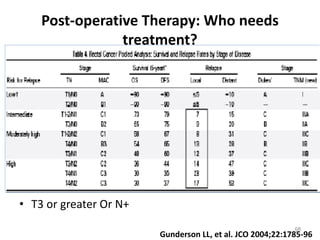
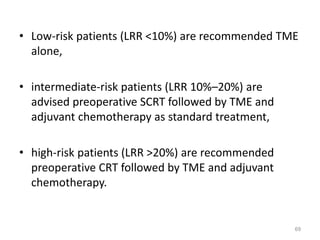
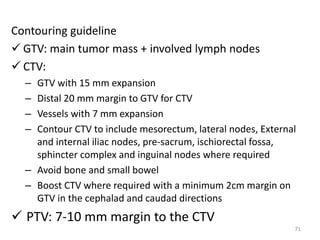
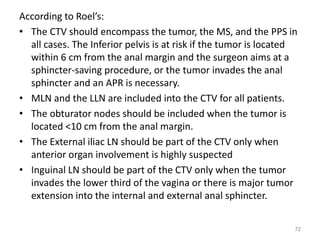
Dr. Ashutosh Mukherji's document discusses contouring for rectal cancers. It provides guidelines for clinical target volume (CTV) delineation based on international consensus. The CTV should encompass the tumor, mesorectum, presacrum, and lymph node regions depending on tumor stage and location. Proper contouring is important for administering precise radiotherapy doses to treat rectal cancer while avoiding unnecessary radiation to healthy tissues.