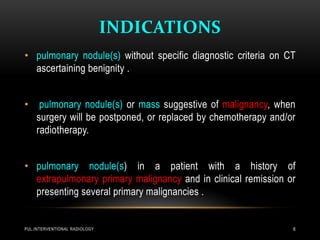
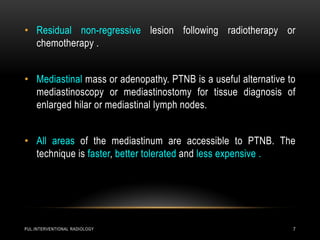
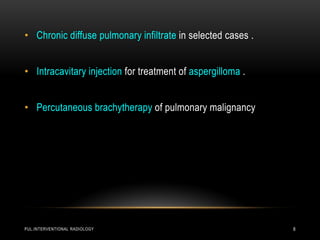
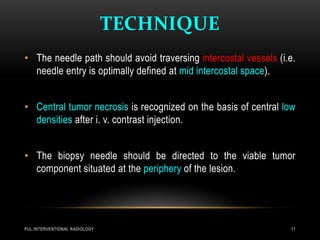
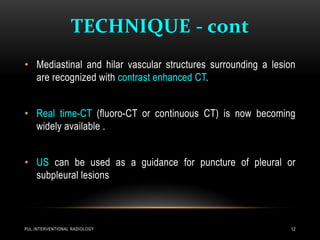
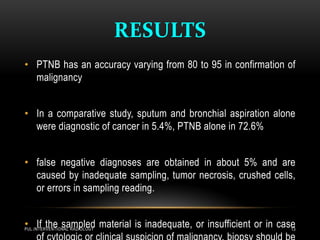
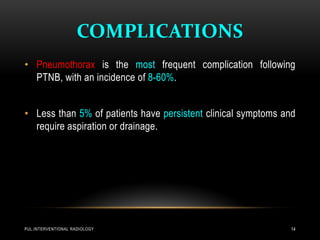
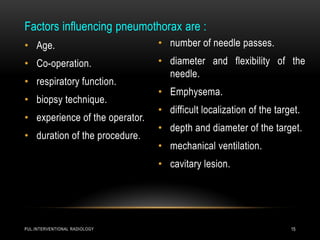
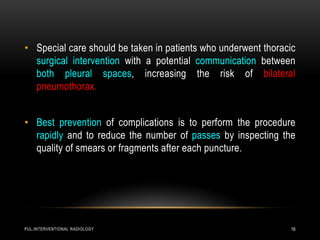
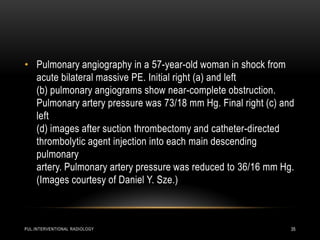
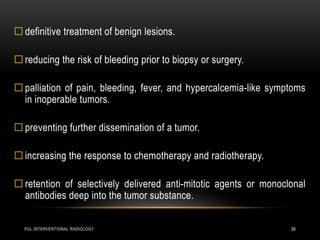
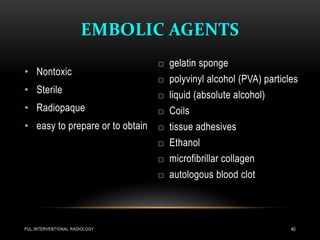
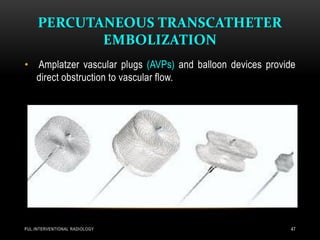
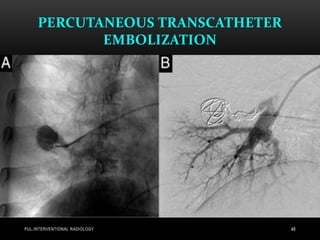
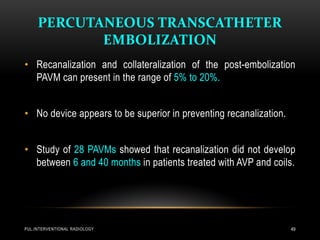
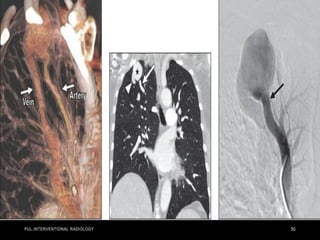
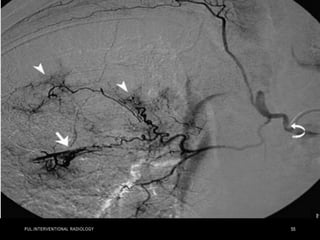
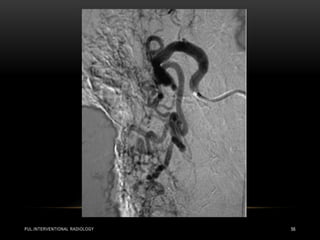
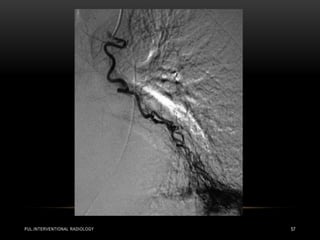
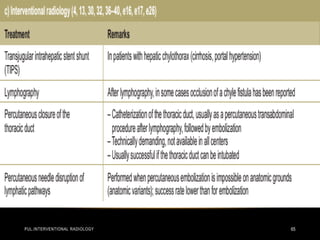
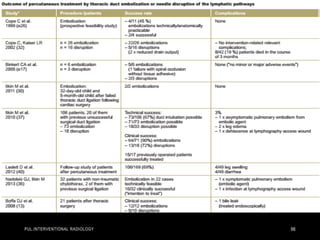
This document discusses pulmonary interventional radiology procedures. It covers percutaneous lung biopsy techniques and indications. Minimally invasive image-guided procedures are described for draining fluid collections in the lungs and chest. Percutaneous transcatheter embolization is discussed as the standard treatment for pulmonary arteriovenous malformations to reduce risks. Various embolic agents, advantages, and recanalization risks are summarized.