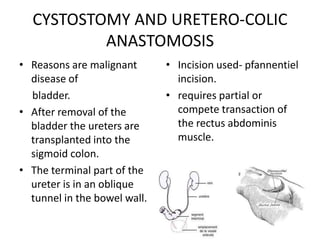
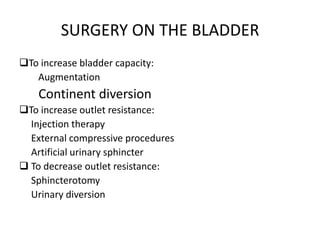
This document provides an overview of physiotherapy for urological surgeries and procedures. It discusses common urological diseases, procedures such as nephrectomy, cystectomy, prostatectomy, and their pre-operative and post-operative physiotherapy. Complications of urological surgeries are also outlined. Physiotherapy focuses on breathing exercises, coughing, range of motion exercises, posture correction, and pelvic floor exercises pre-operatively and post-operatively to aid recovery.