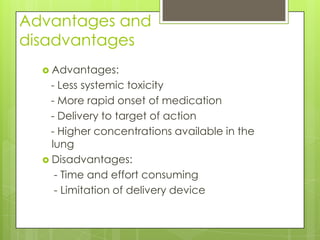
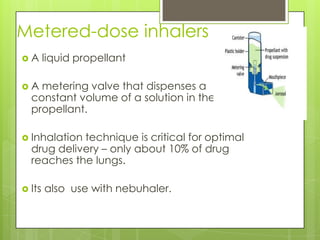
Inhalation is the administration of drugs through the nasal or oral respiratory route. It has several advantages over other routes of administration including lower systemic toxicity, more rapid onset of action, and higher drug concentrations delivered directly to the target site in the lungs. Common conditions treated with inhalation therapy include asthma, chronic bronchitis, and emphysema. There are various types of inhalation devices that deliver drugs to the lungs including metered dose inhalers, dry powder inhalers, nebulizers, and spacers. Proper inhalation technique is important for optimal drug delivery to the lungs from these devices.

![18
Some Disadvantages of Jet
Nebulizers
Less portable than inhalers
Requires power
source, maintenance, and cleaning
Output is device dependent
Delivery may take 5 to 10 minutes or
longer
O’Donohue et al. Chest. 1996;109:814-820; Dolovich et al. Chest. 2005;127:335-376; Pulmicort
Respules 0.25 and 0.5 mg [package insert]. Wilmington, DE: AstraZeneca LP, 6/2005. NAEPP.
Publication no. 97-4051.](https://image.slidesharecdn.com/inhalationtherapy-120807161343-phpapp02/85/Inhalation-therapy-18-320.jpg)