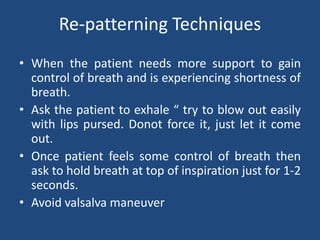
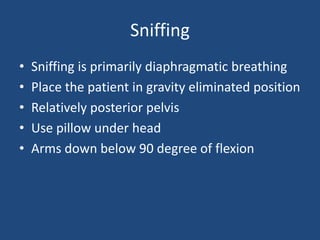
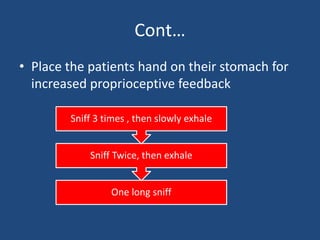
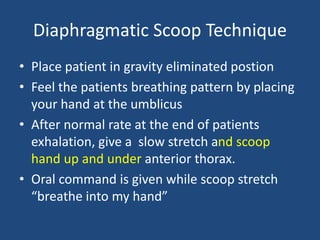
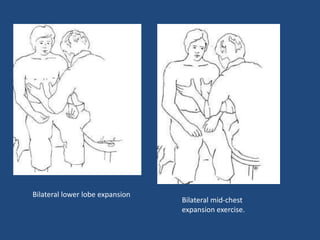
The document discusses diaphragm facilitation techniques aimed at improving breathing patterns in patients with respiratory issues, particularly post-surgery or due to neurological dysfunction. It outlines various methods for enhancing diaphragmatic breathing and managing accessory muscle use, emphasizing the importance of patient positioning and relaxation techniques. Strategies such as sniffing, lateral costal breathing, and upper chest inhibition are detailed to aid in effective ventilation and rehabilitation.