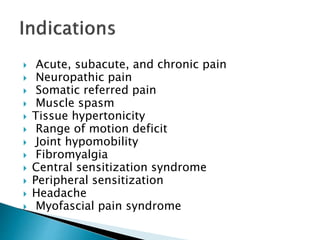
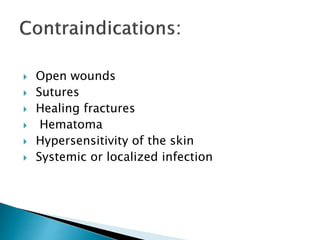
Positional Release Therapy (PRT) is a therapeutic technique that resolves somatic dysfunction by placing the body in a position of comfort, alleviating pain through the unwinding of knotted tissues. The method involves identifying tender points and applying treatment that lasts varying durations for orthopedic and neurologic patients, aiming to normalize muscle tone, reduce joint stiffness, and improve circulation. The ultimate goal of PRT is to achieve optimal relaxation of involved tissues, leading to pain relief and enhanced mobility.