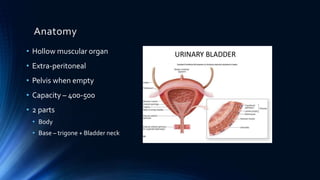
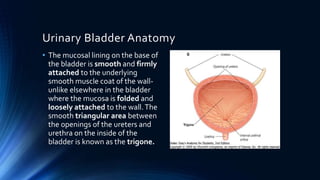
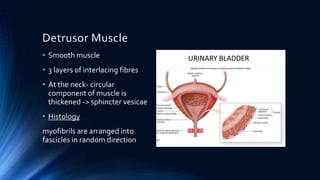
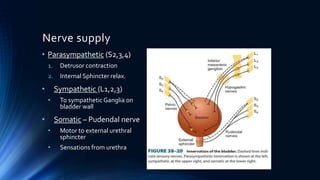
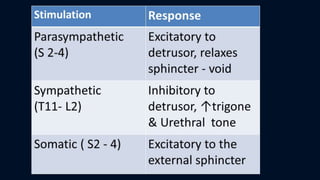
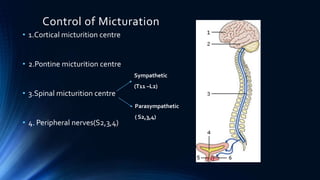
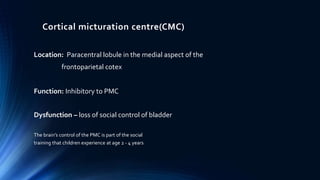
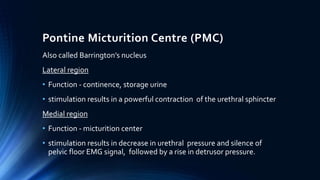
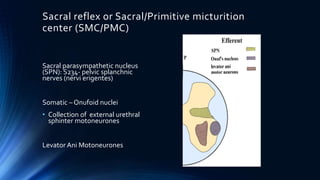
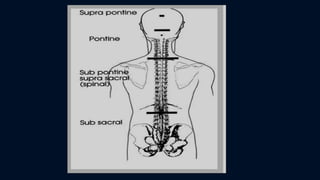
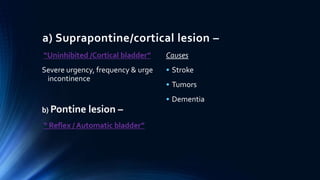
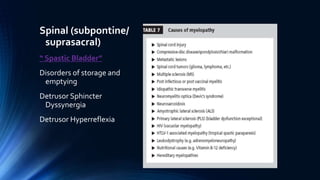
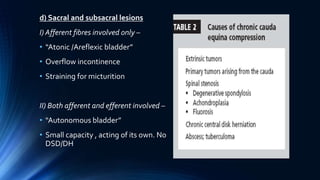
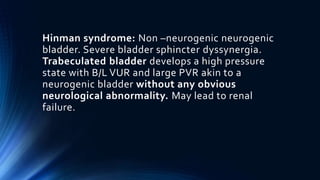
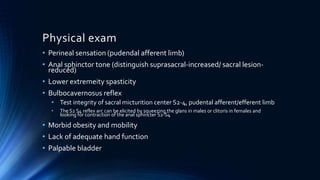
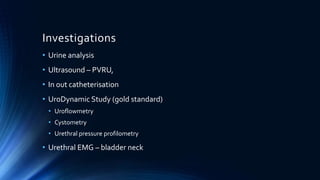
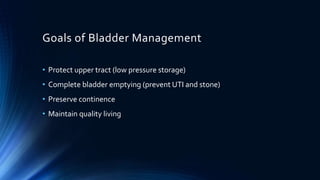
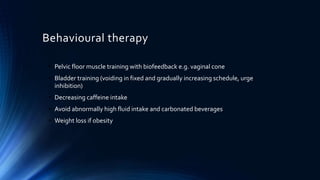
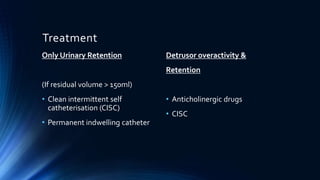
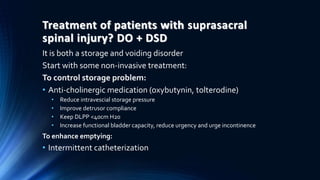
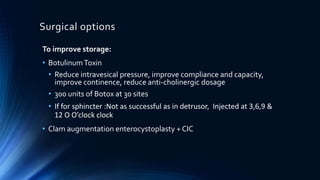
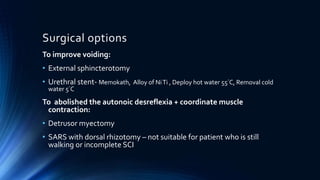
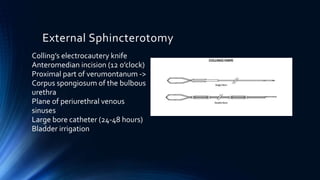
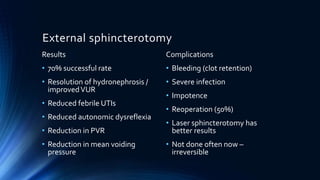
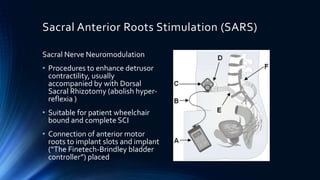
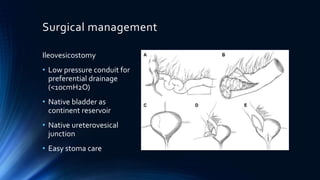
This document discusses neurogenic bladder, which occurs due to neurological dysfunction or insult to the nervous system. It describes the anatomy and functions of the normal bladder, as well as the different types of neurogenic bladder based on the level of neurological insult (e.g. suprapontine, pontine, spinal). Treatment options are discussed, including behavioral therapies, medications, injections, surgeries and procedures like clean intermittent catheterization and sacral anterior root stimulation. The goals of bladder management and treatment considerations for different types of neurogenic bladder are also summarized.