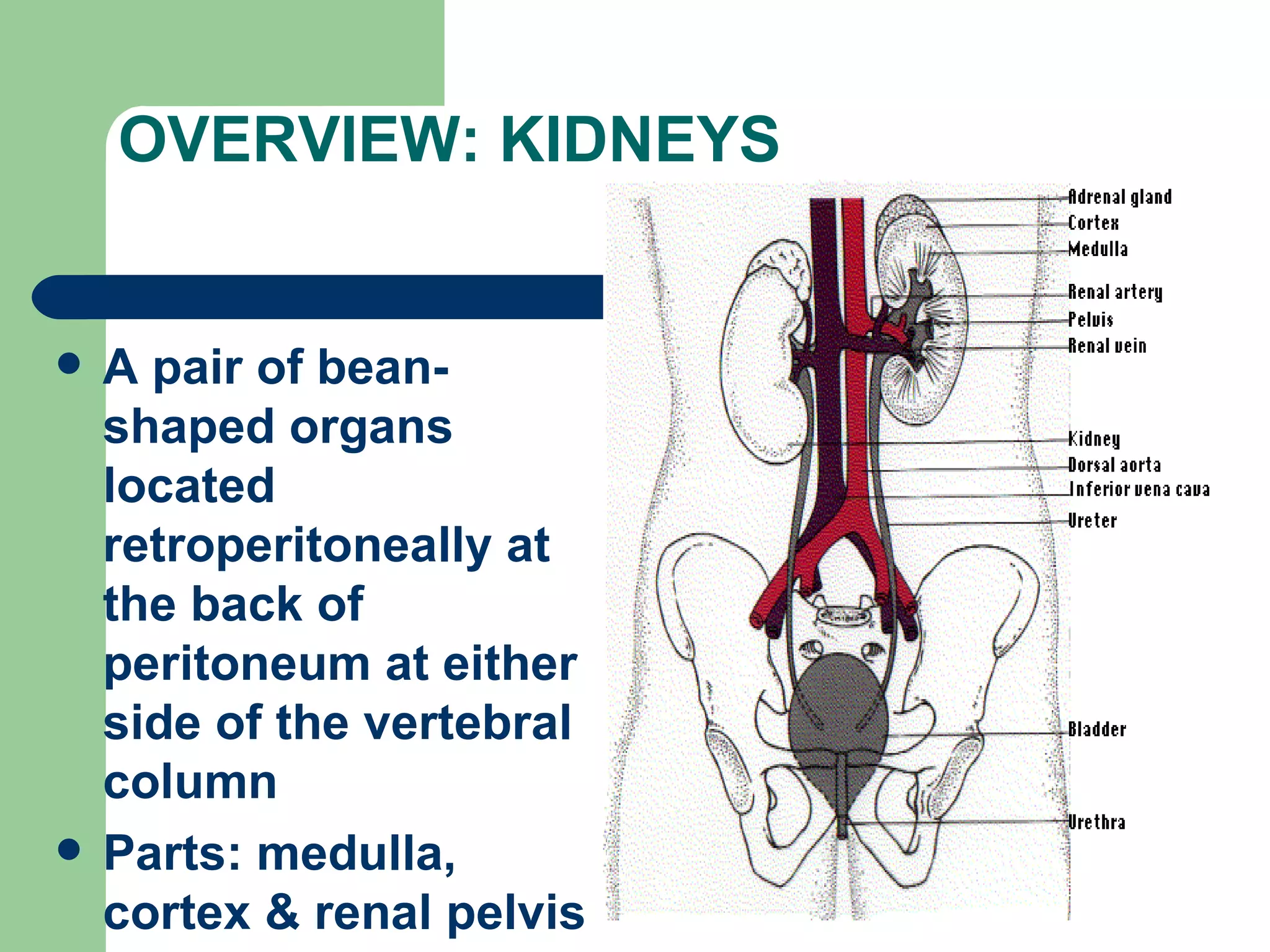
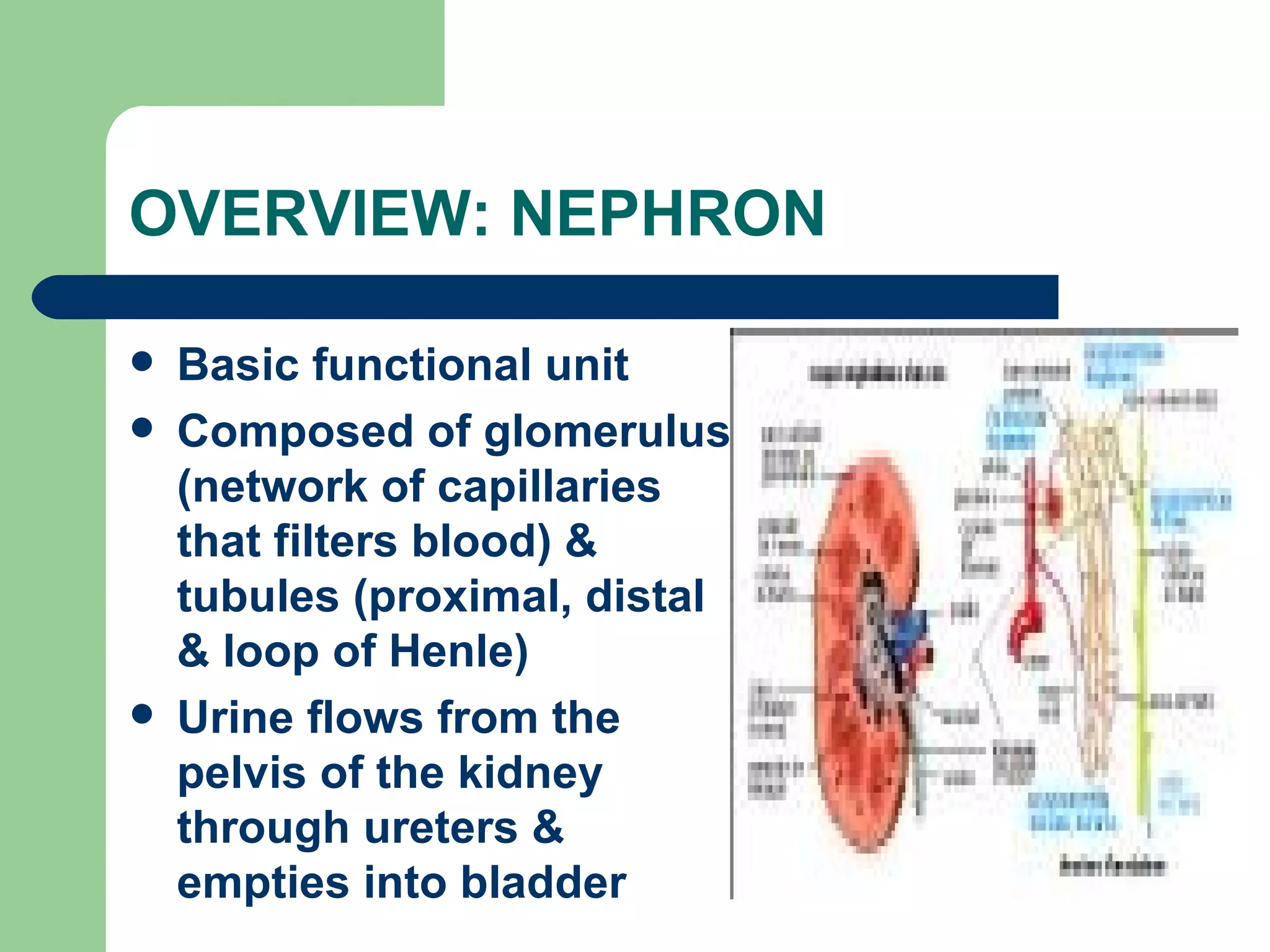
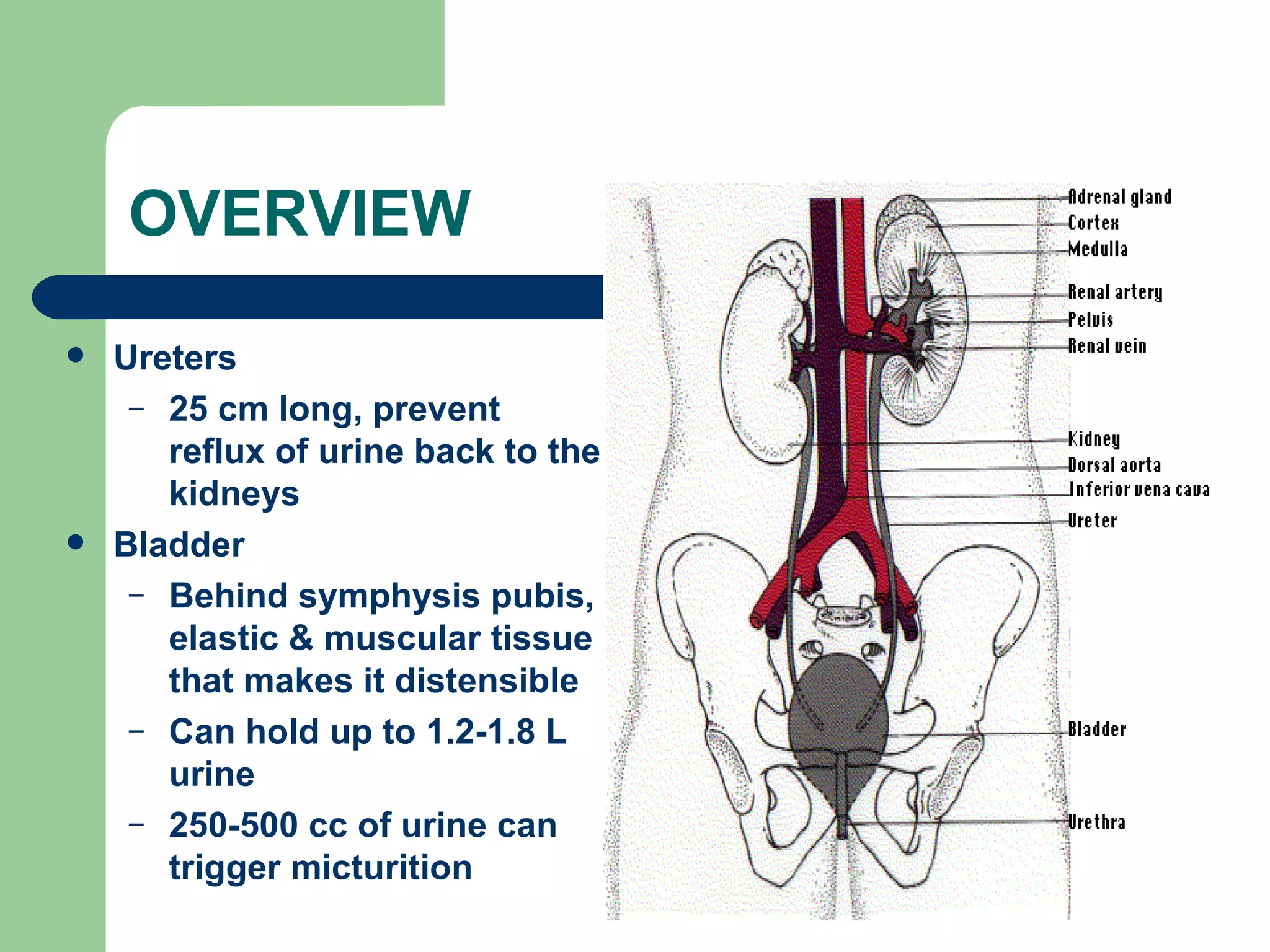
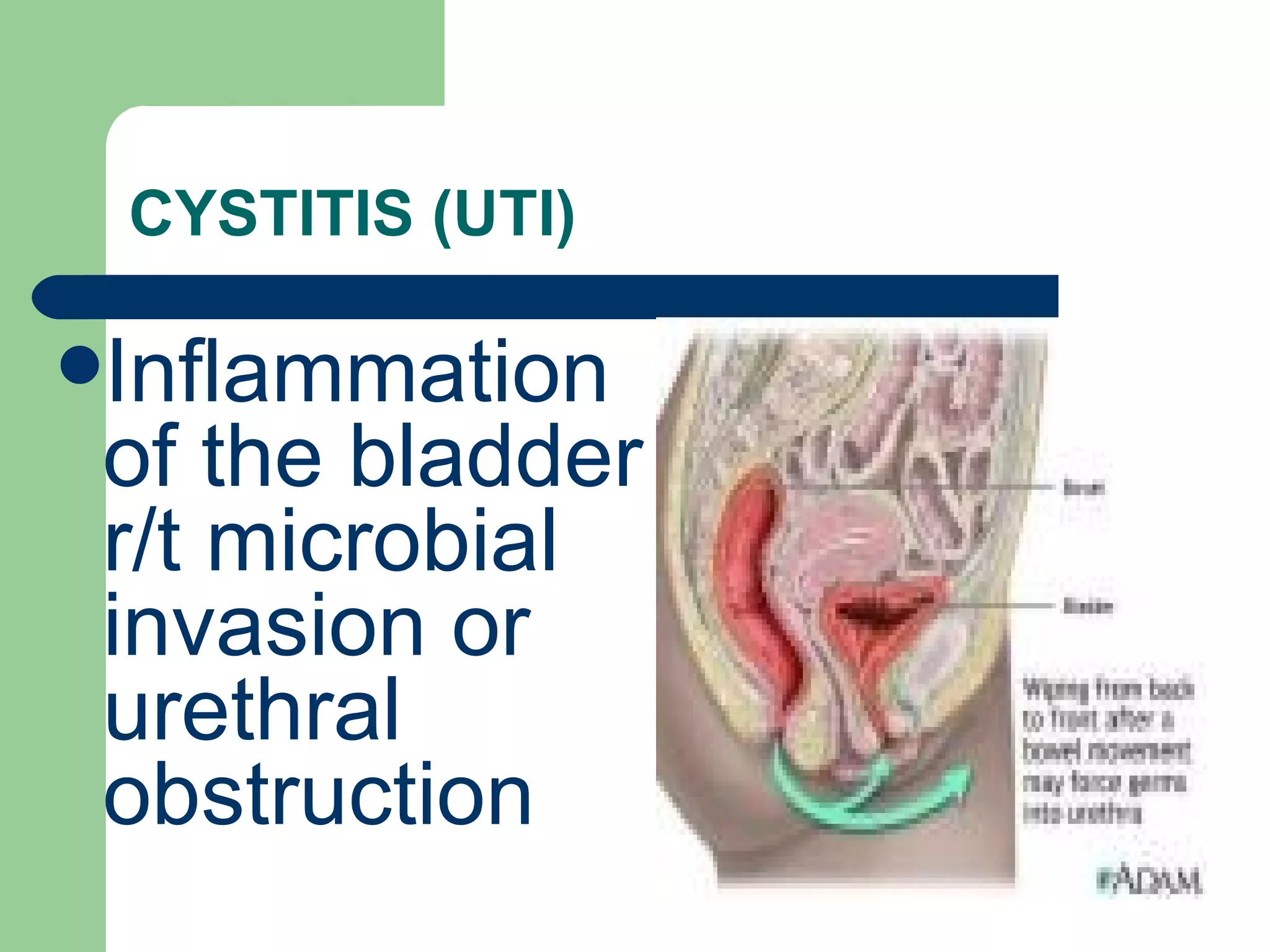
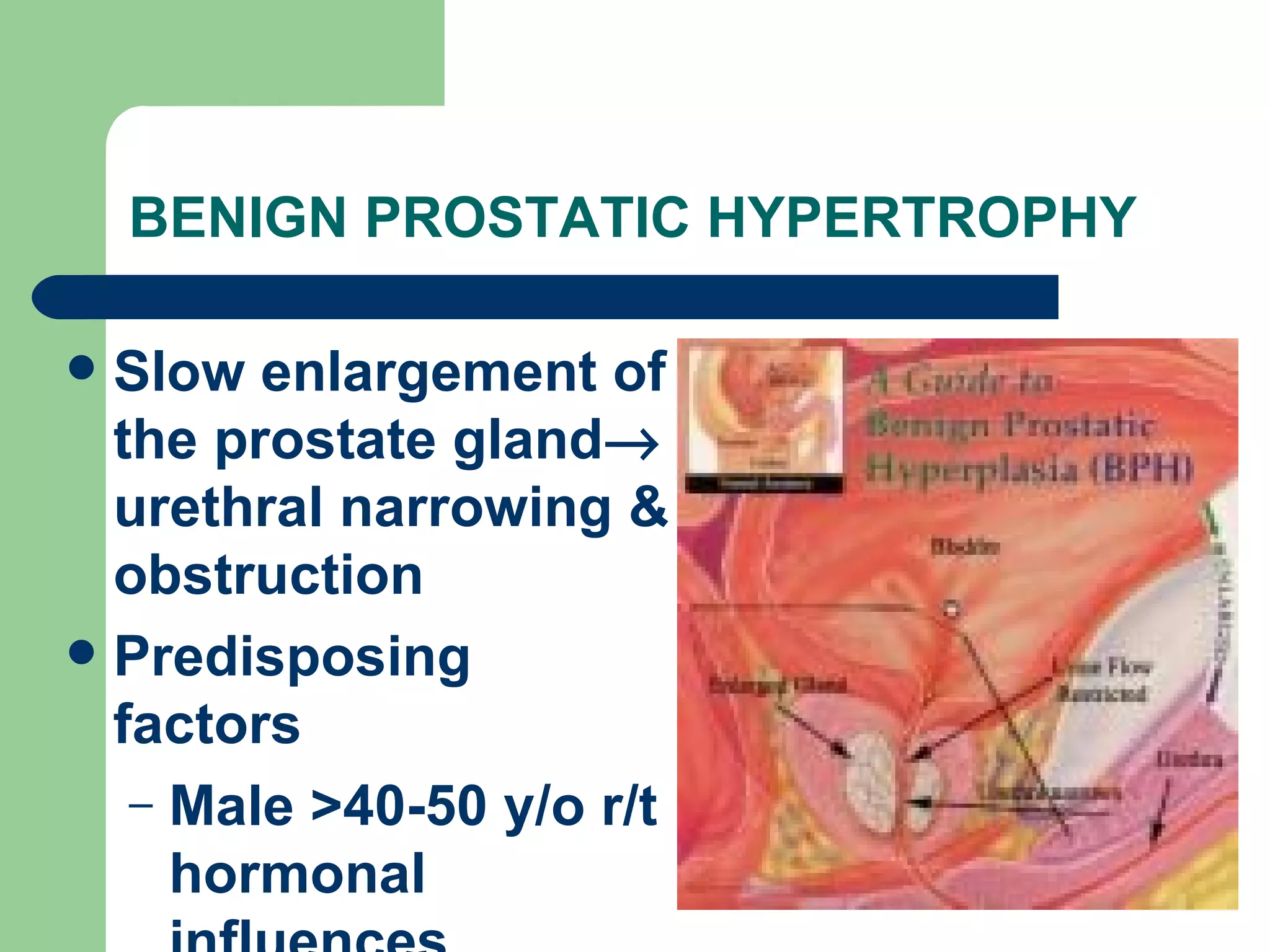
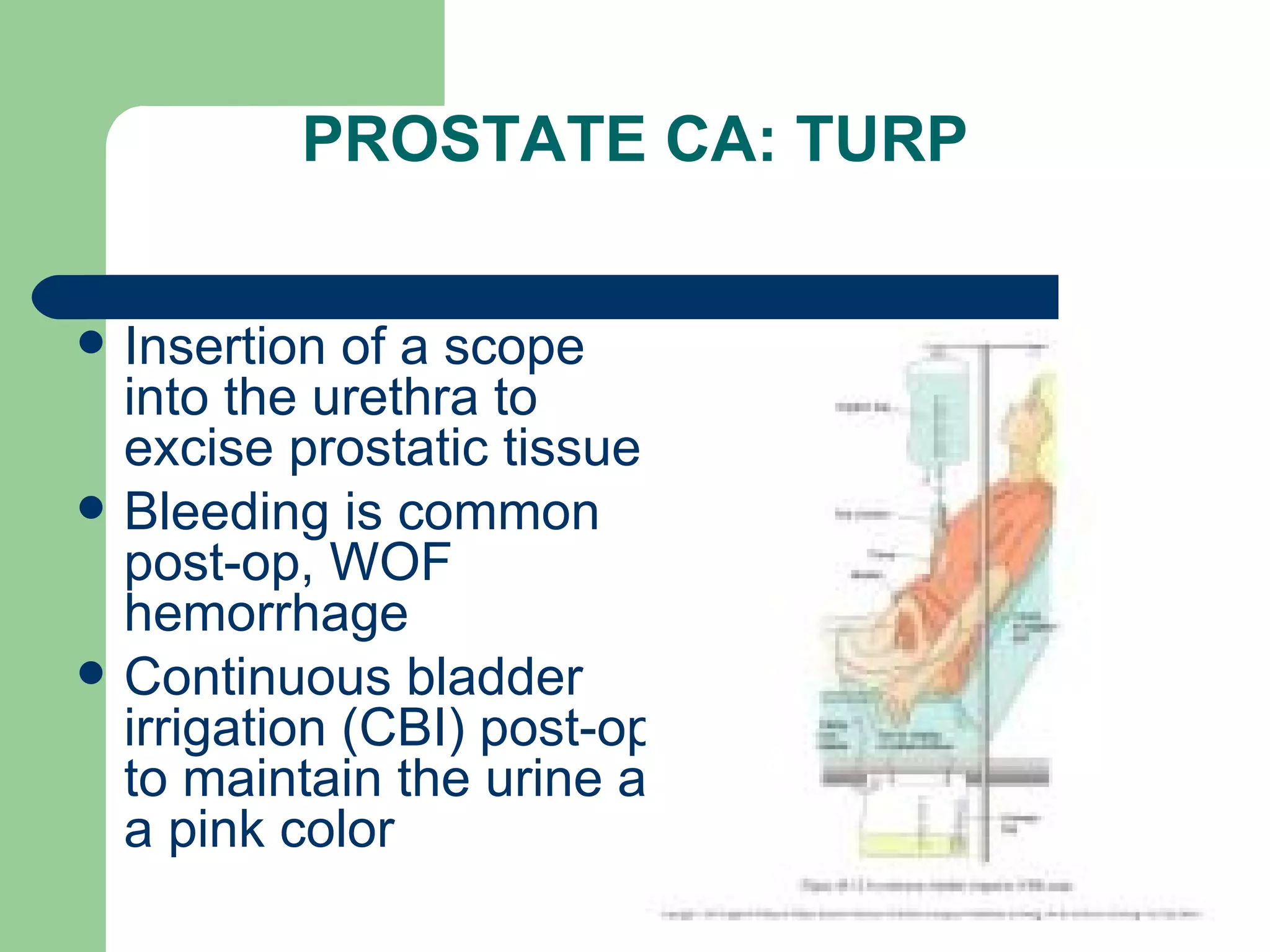
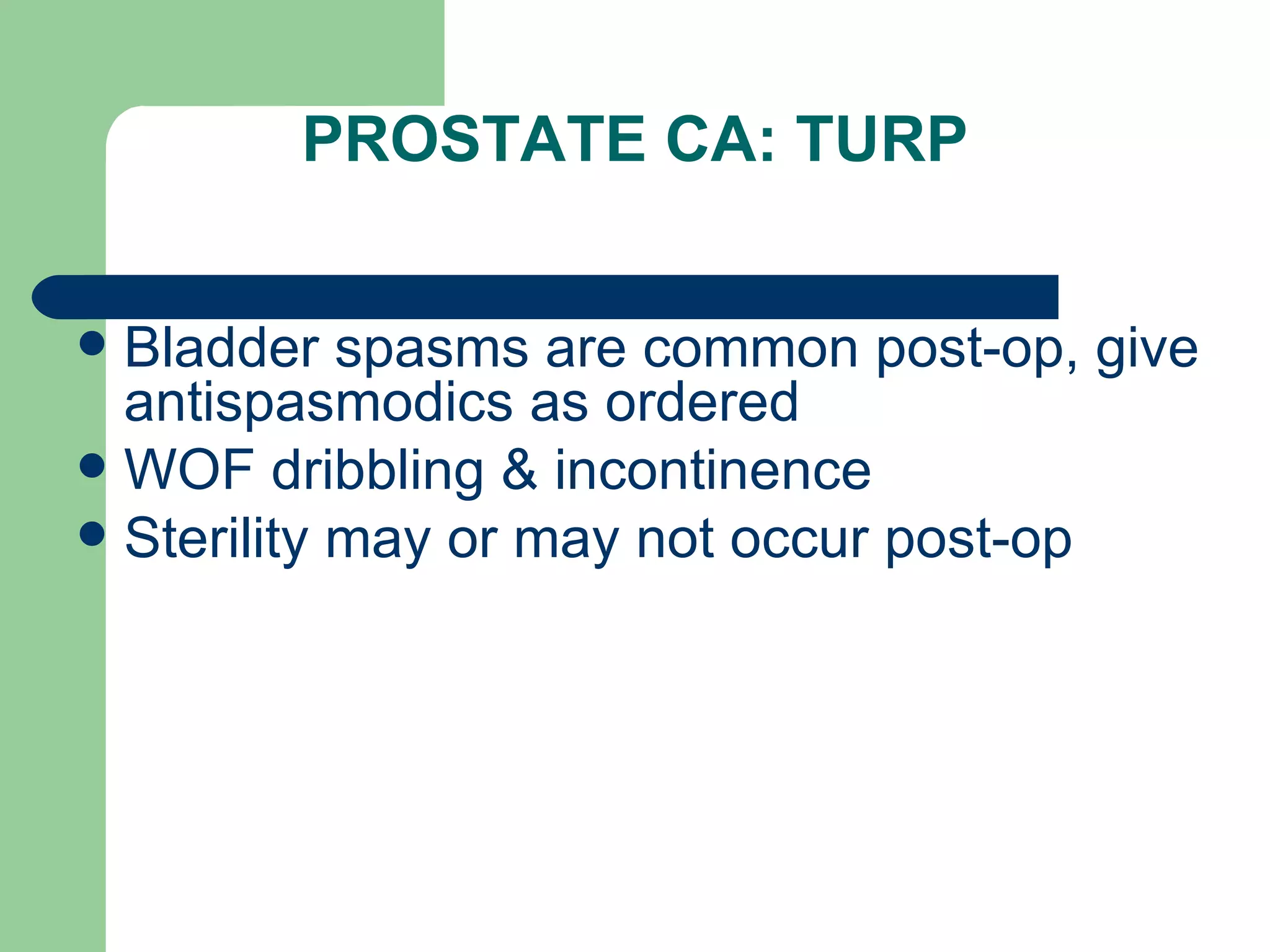
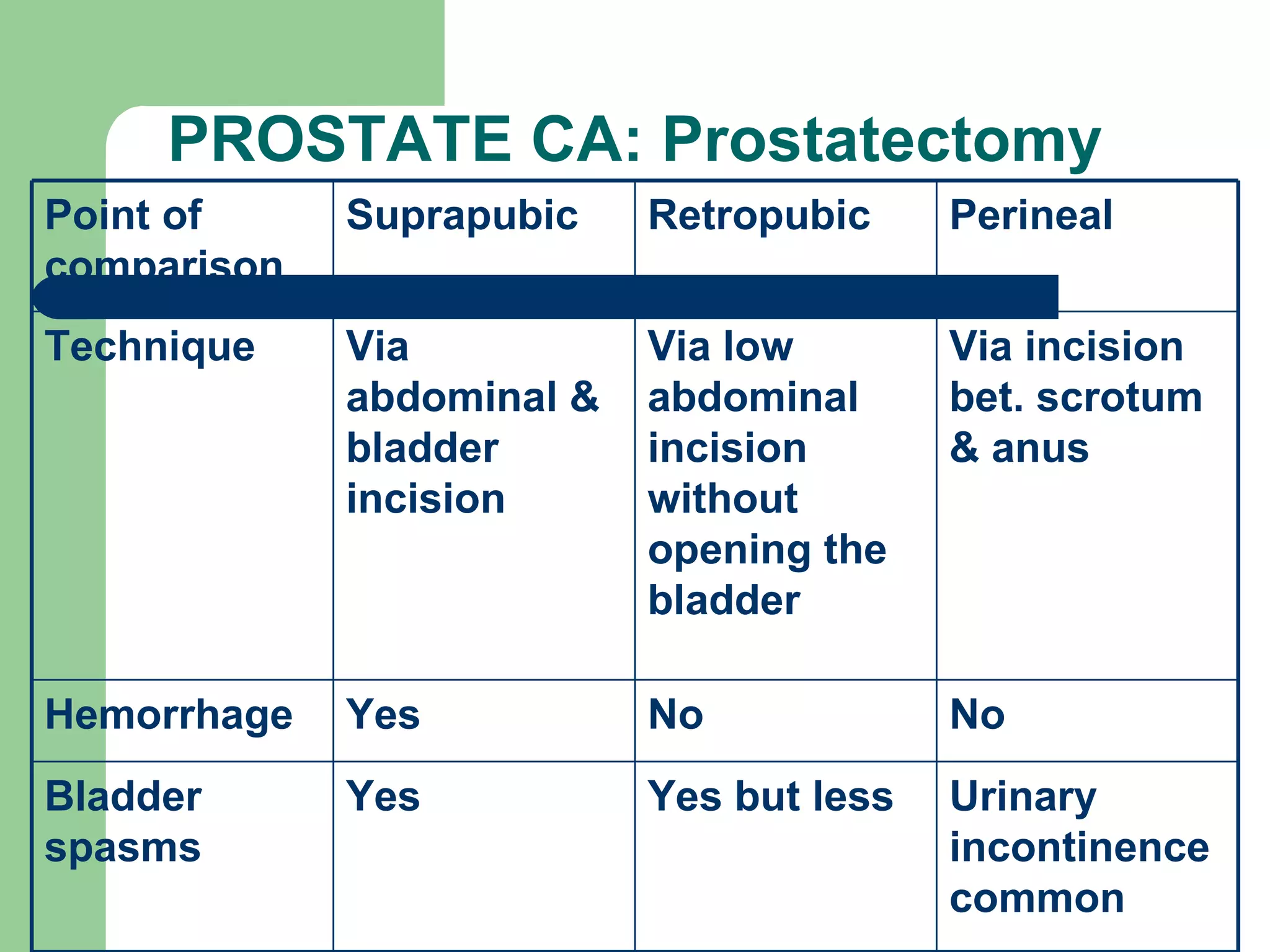
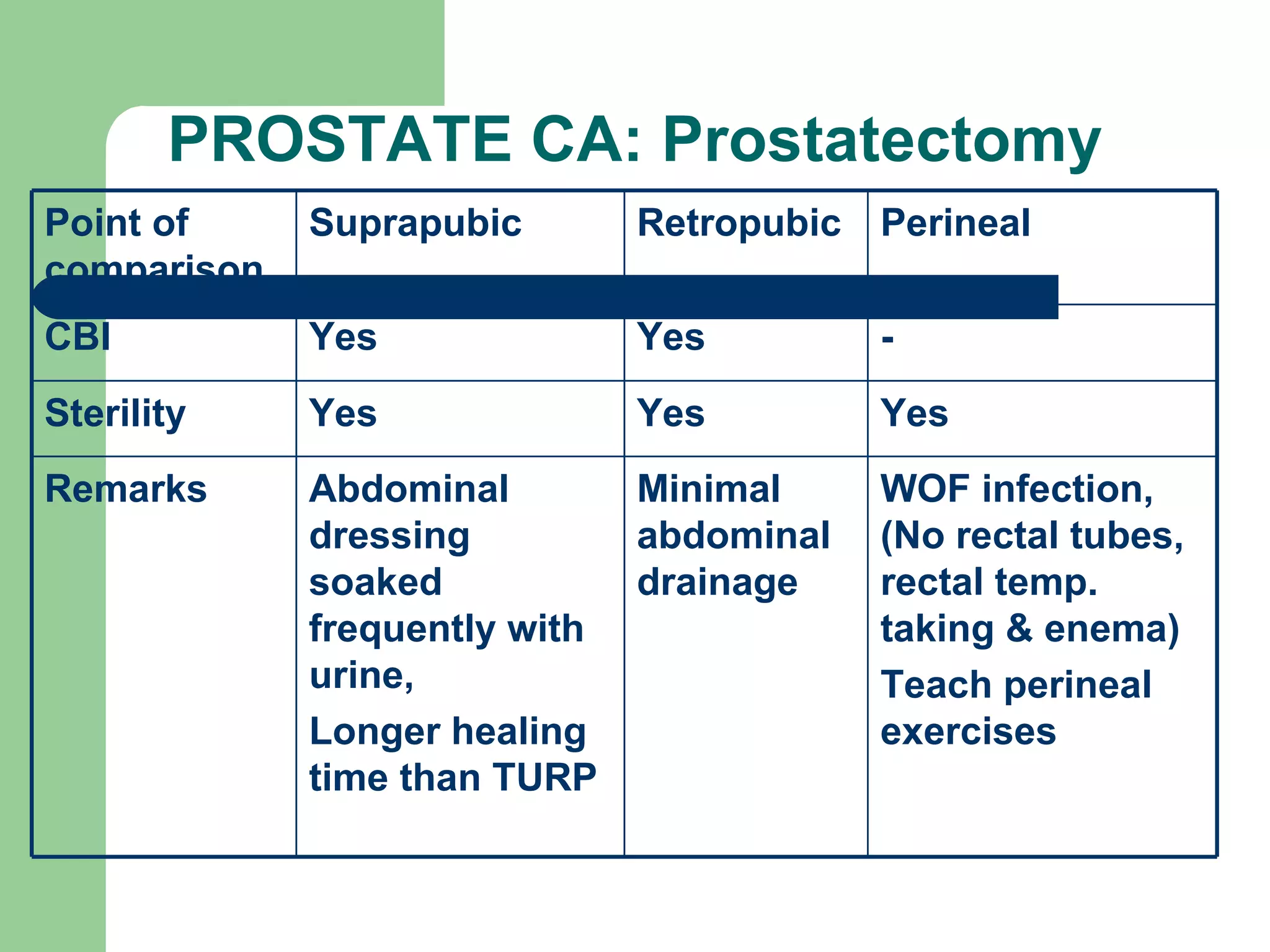
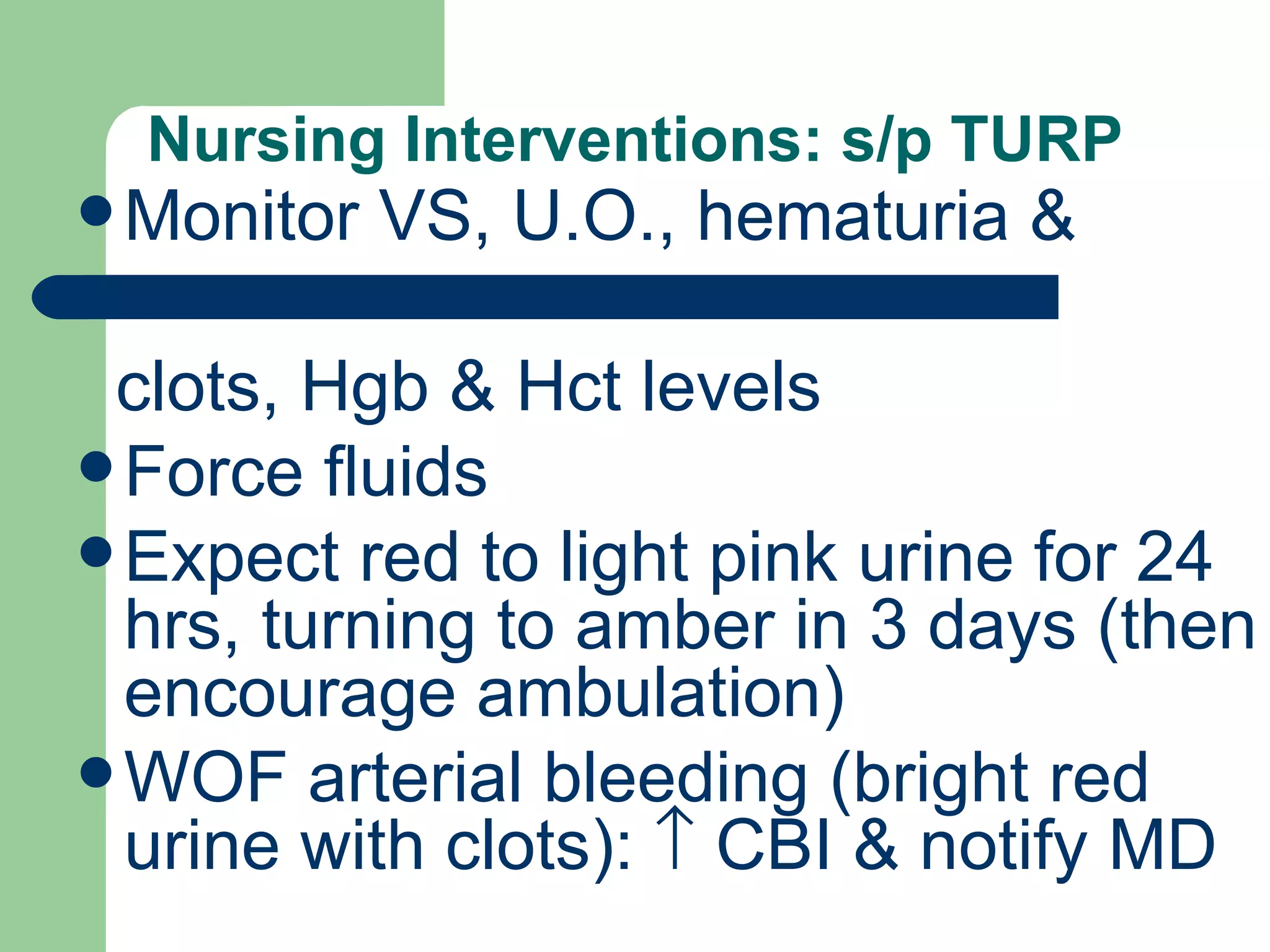
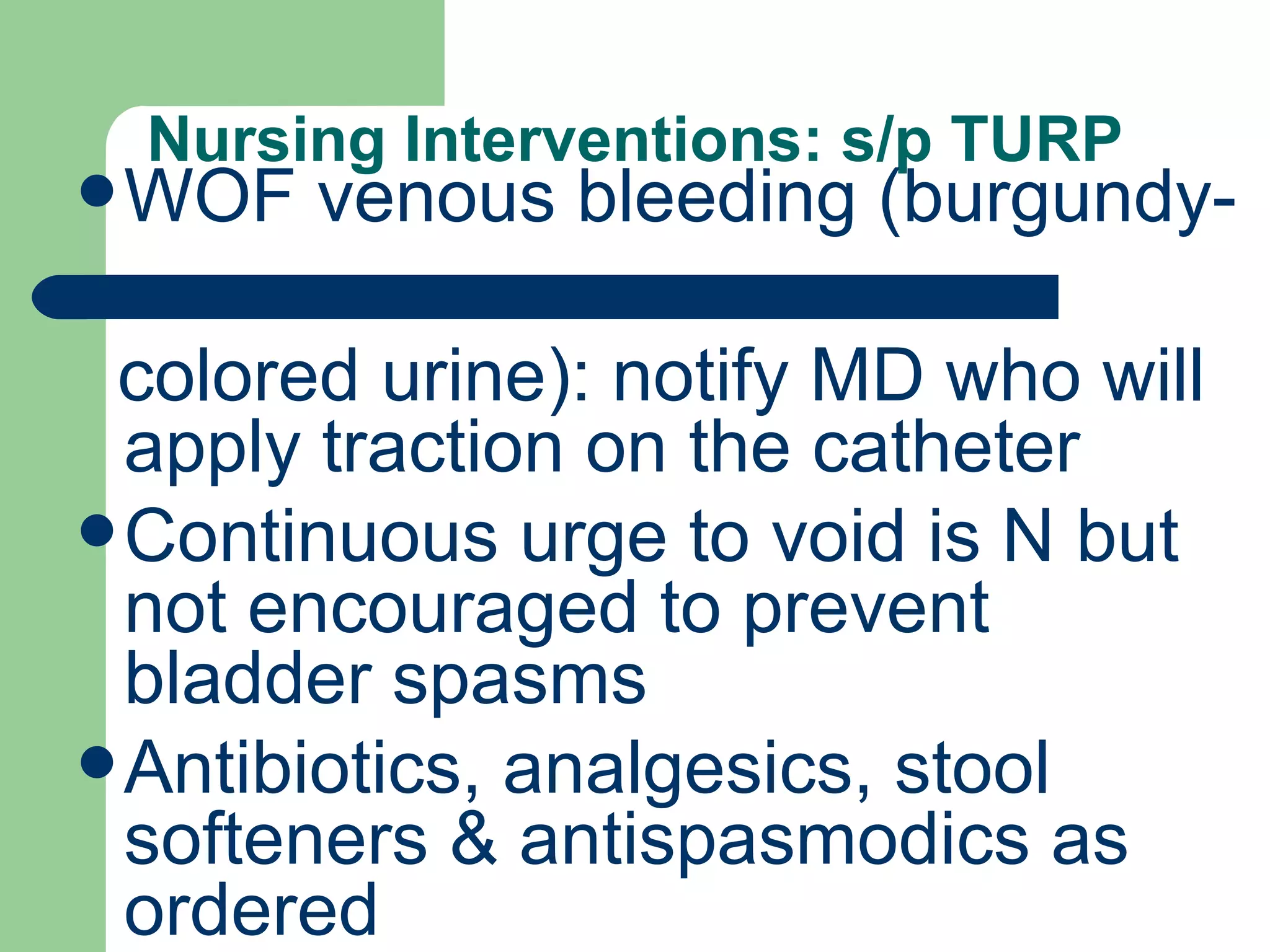
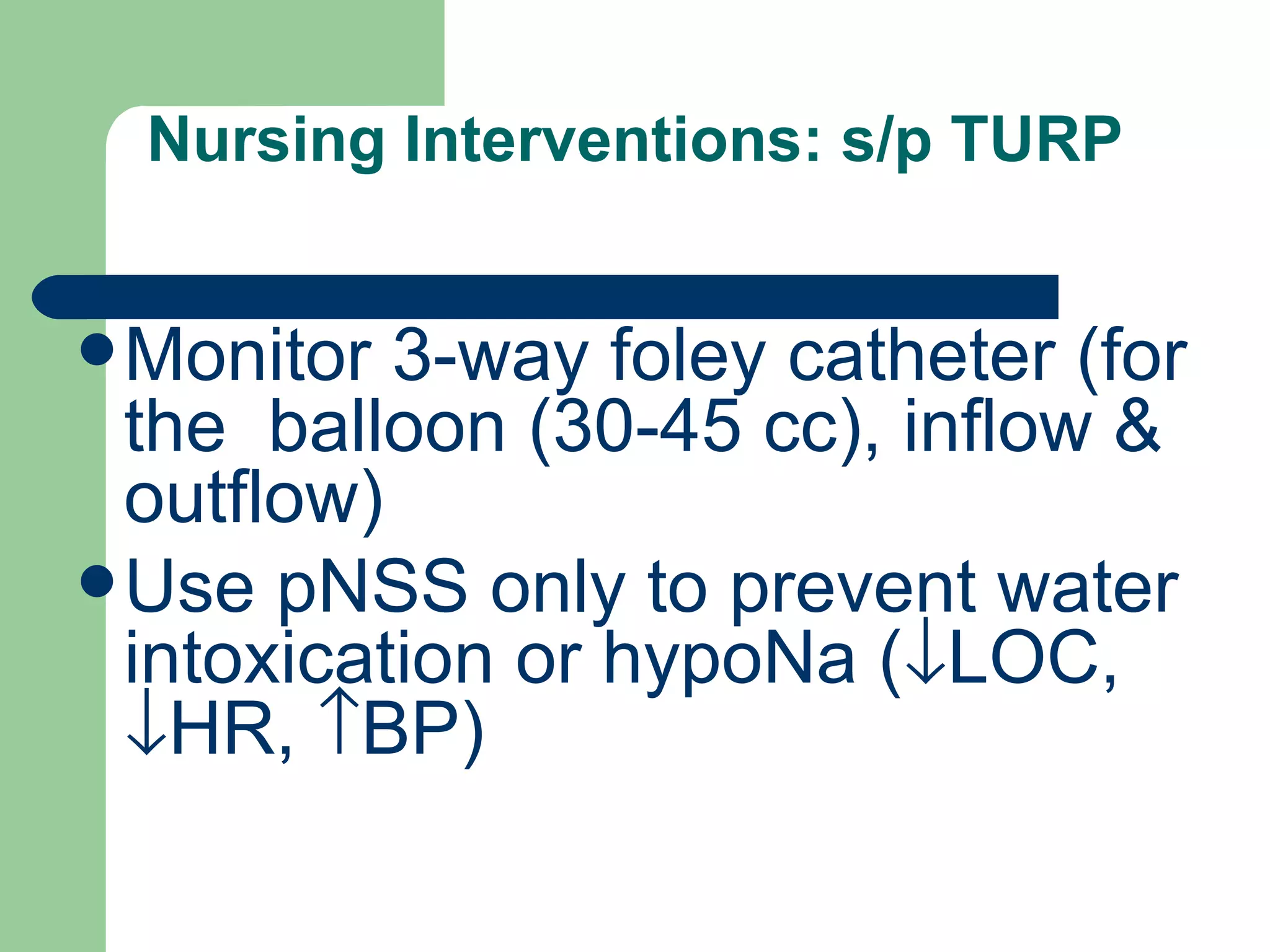
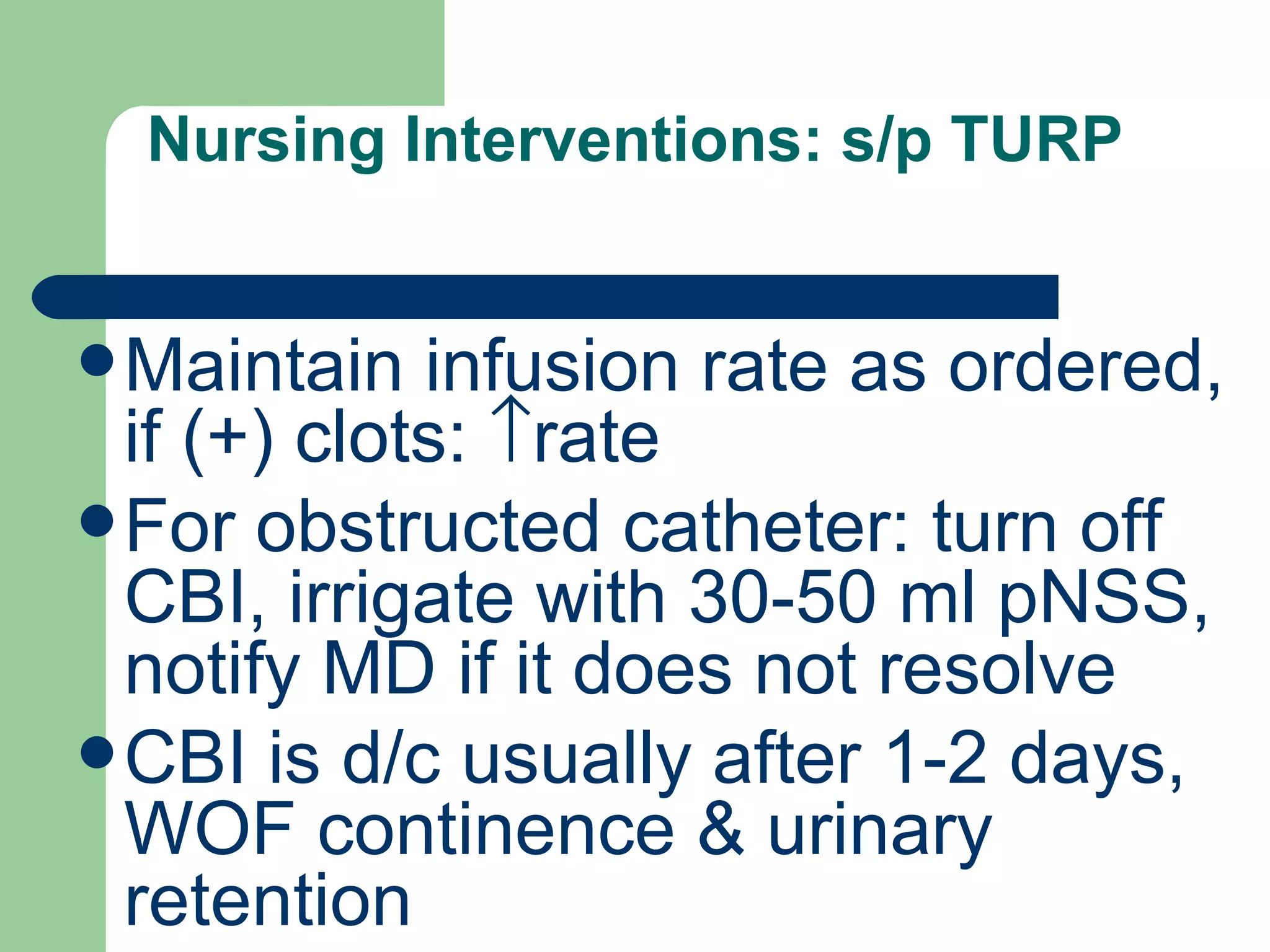
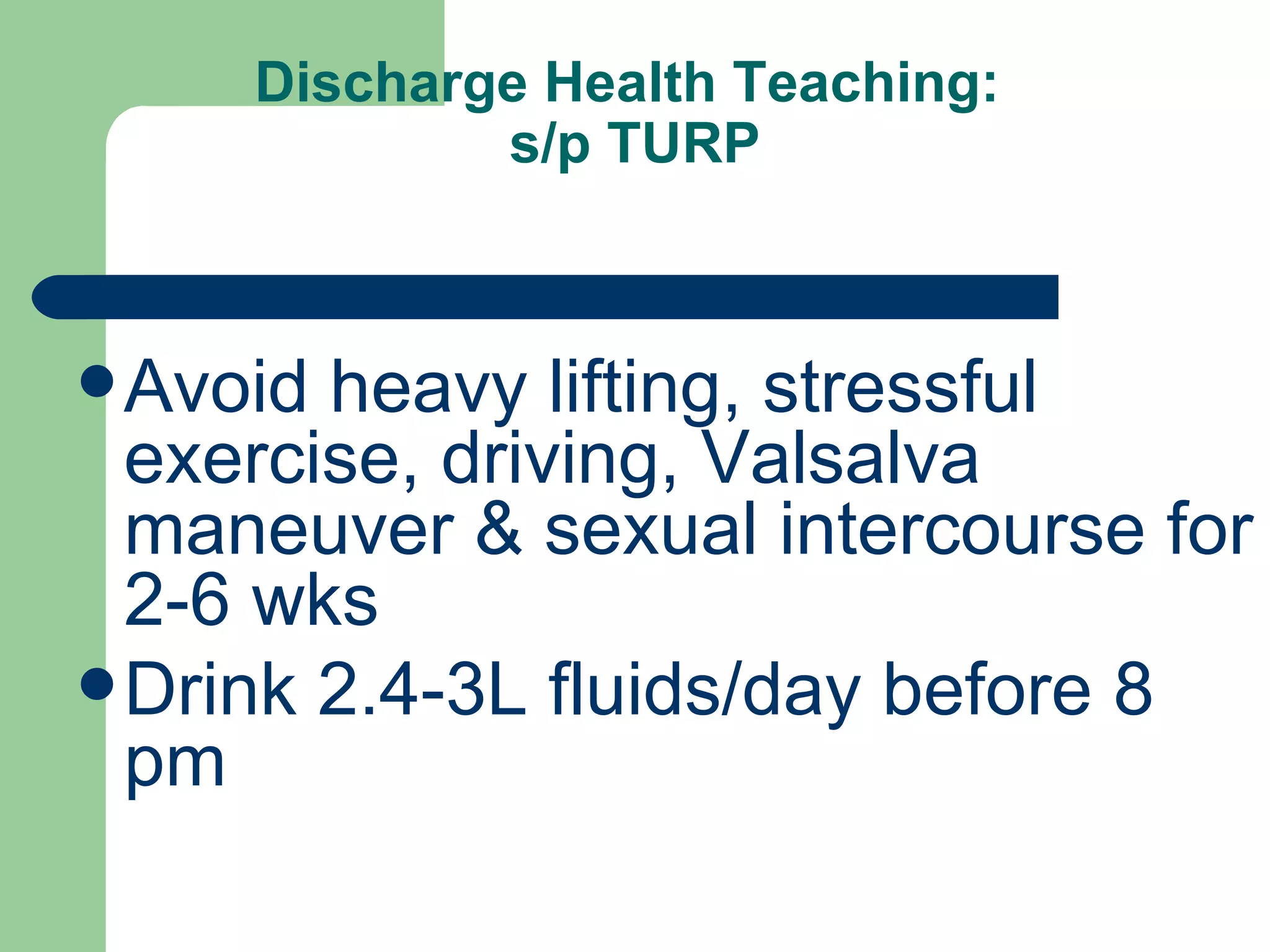
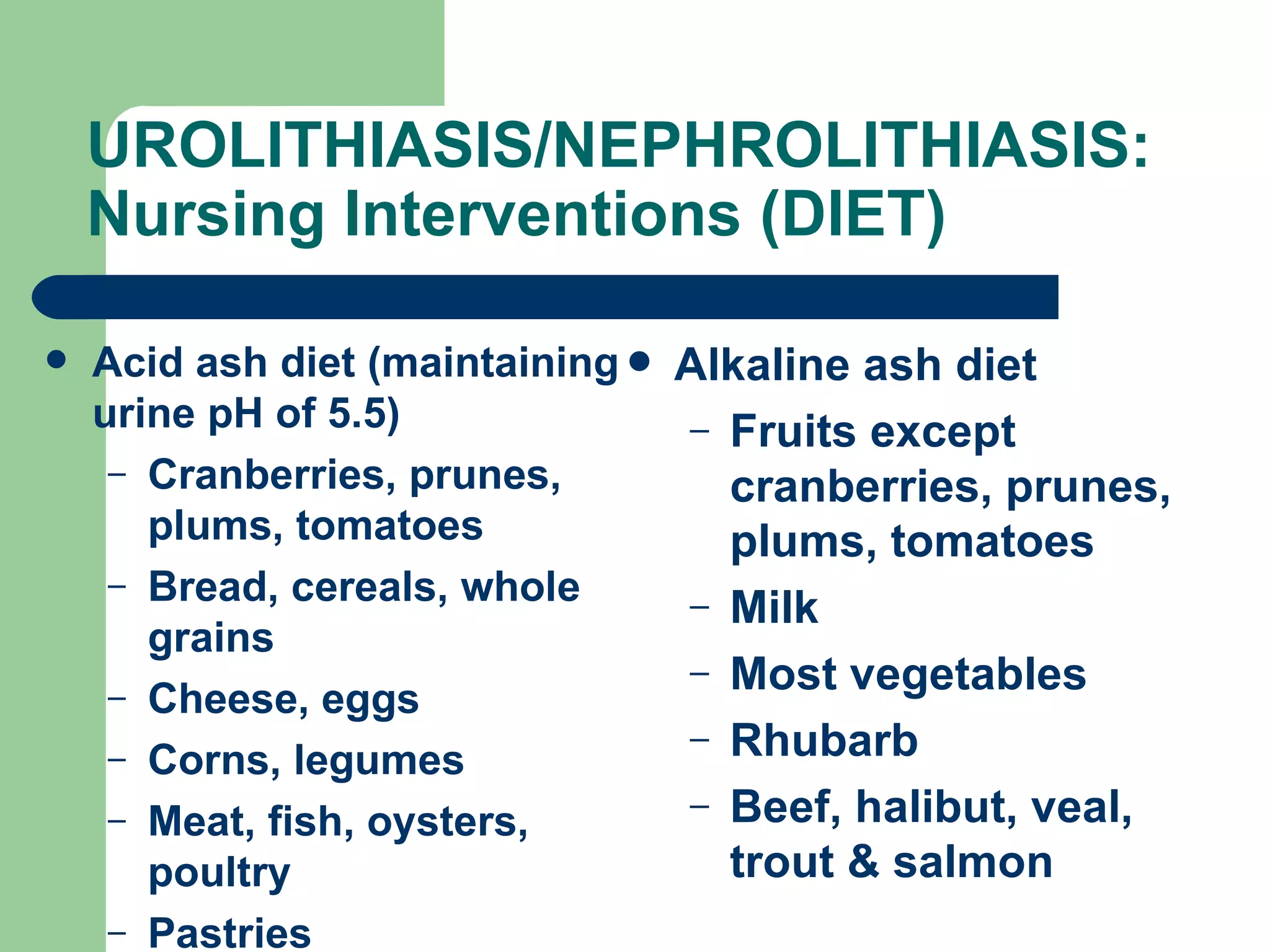
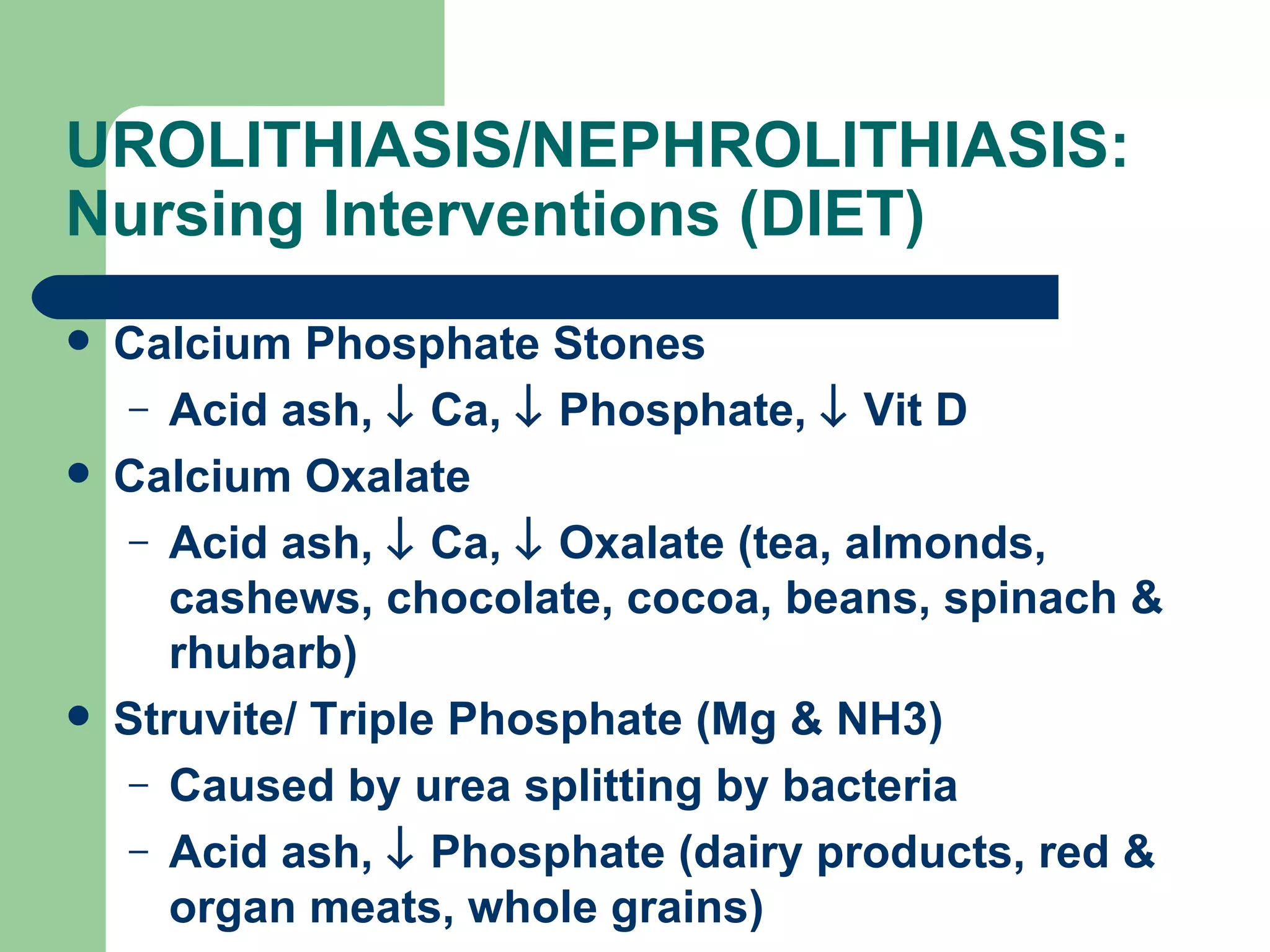
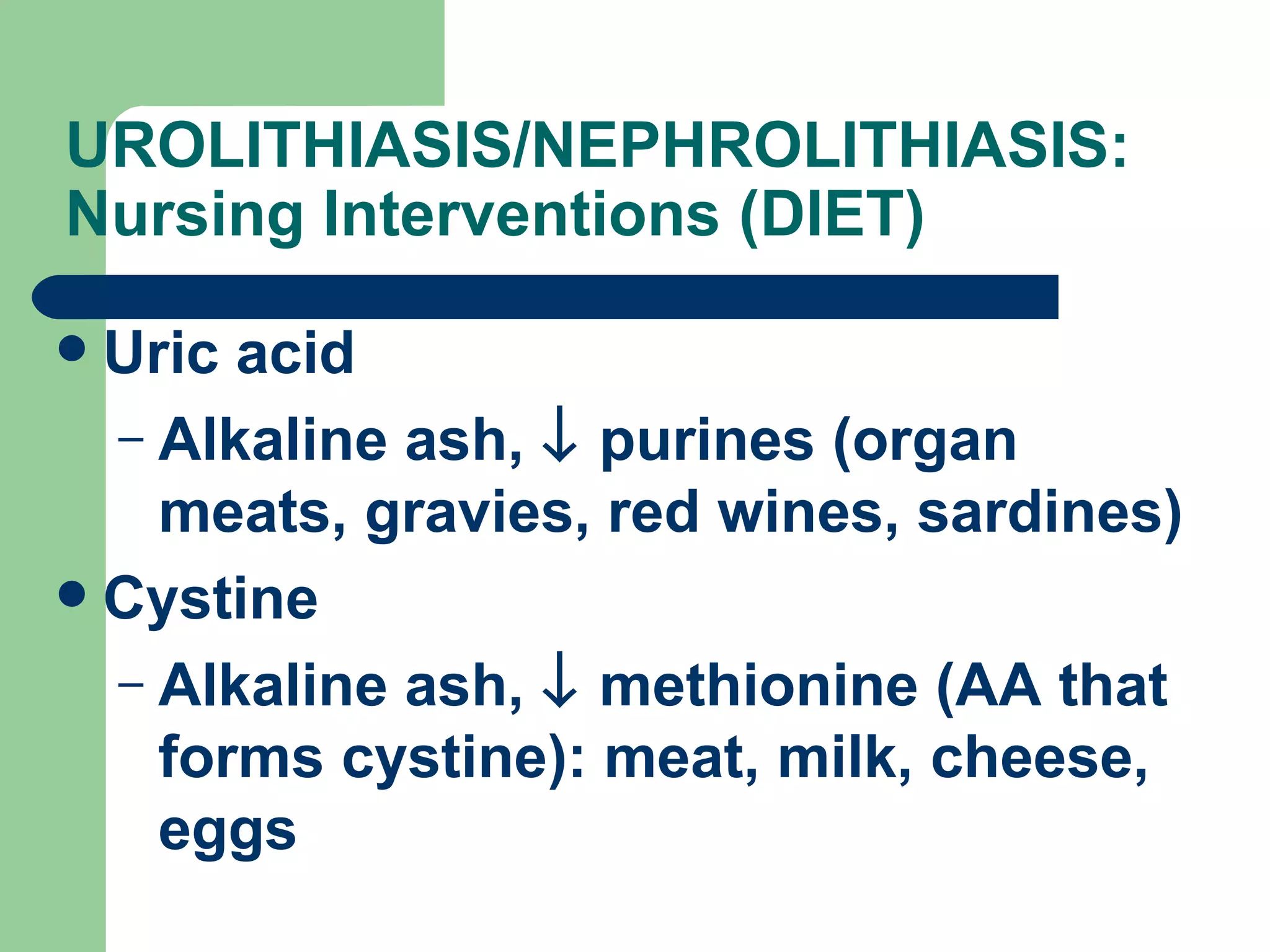
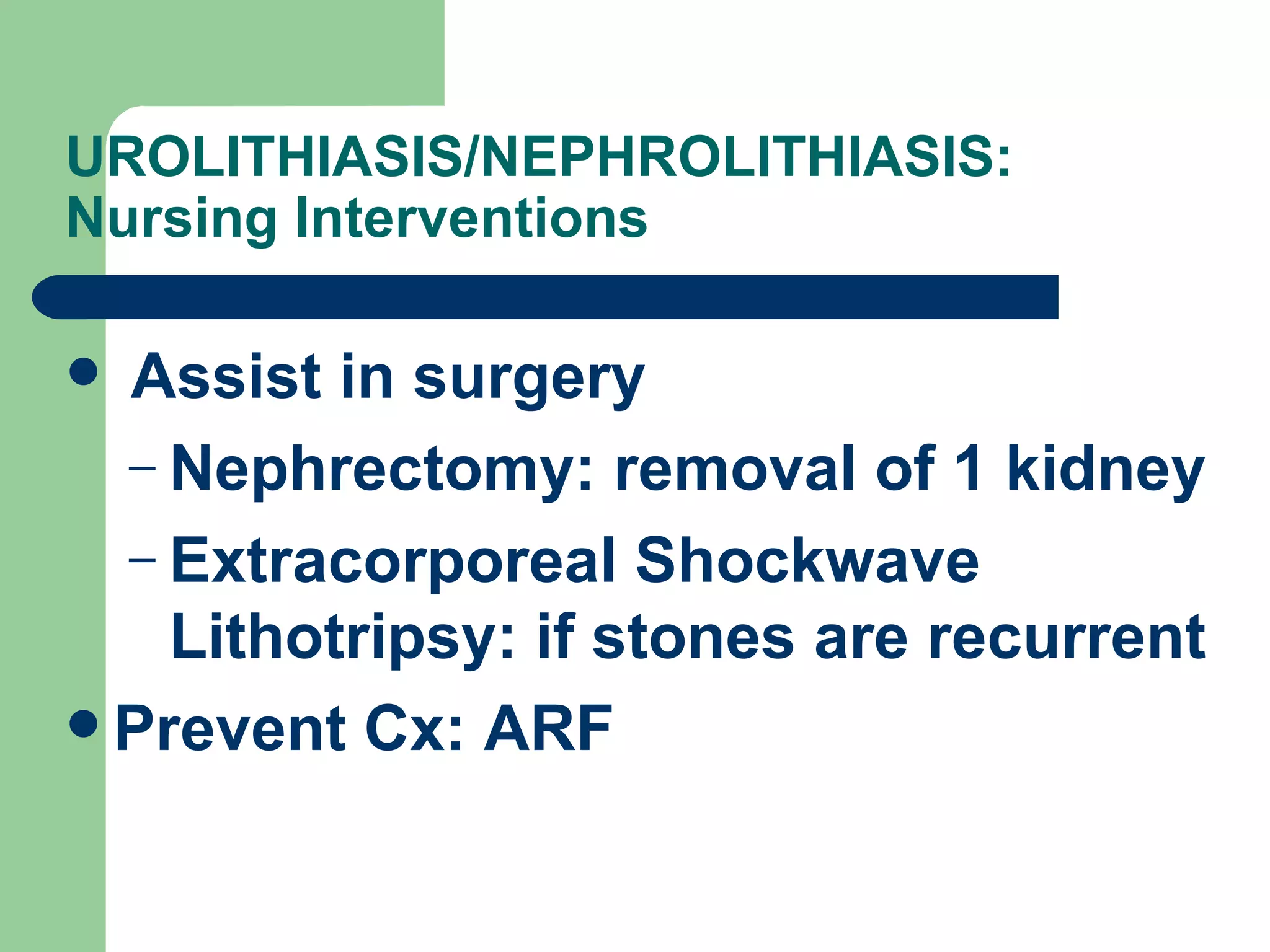
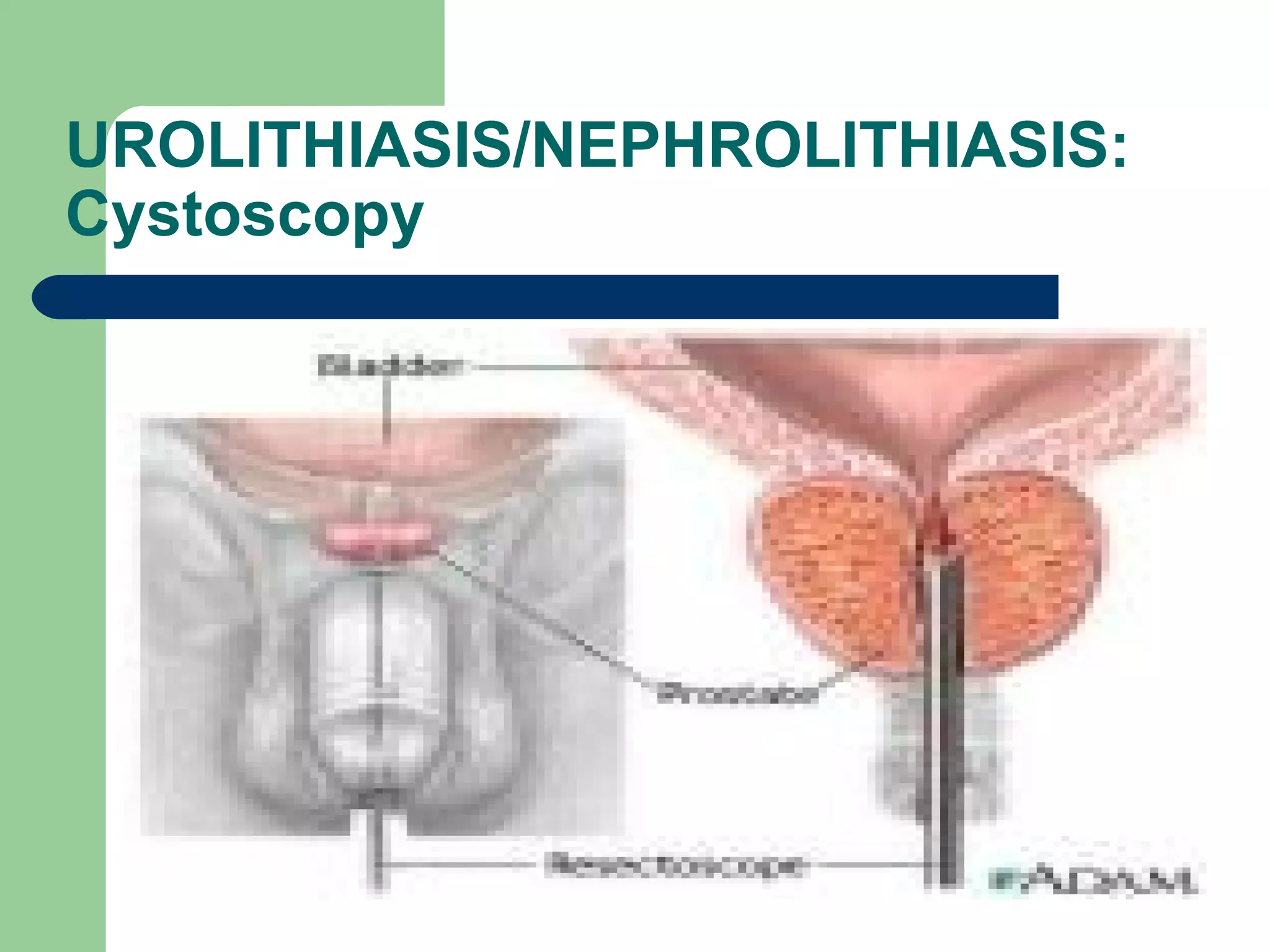
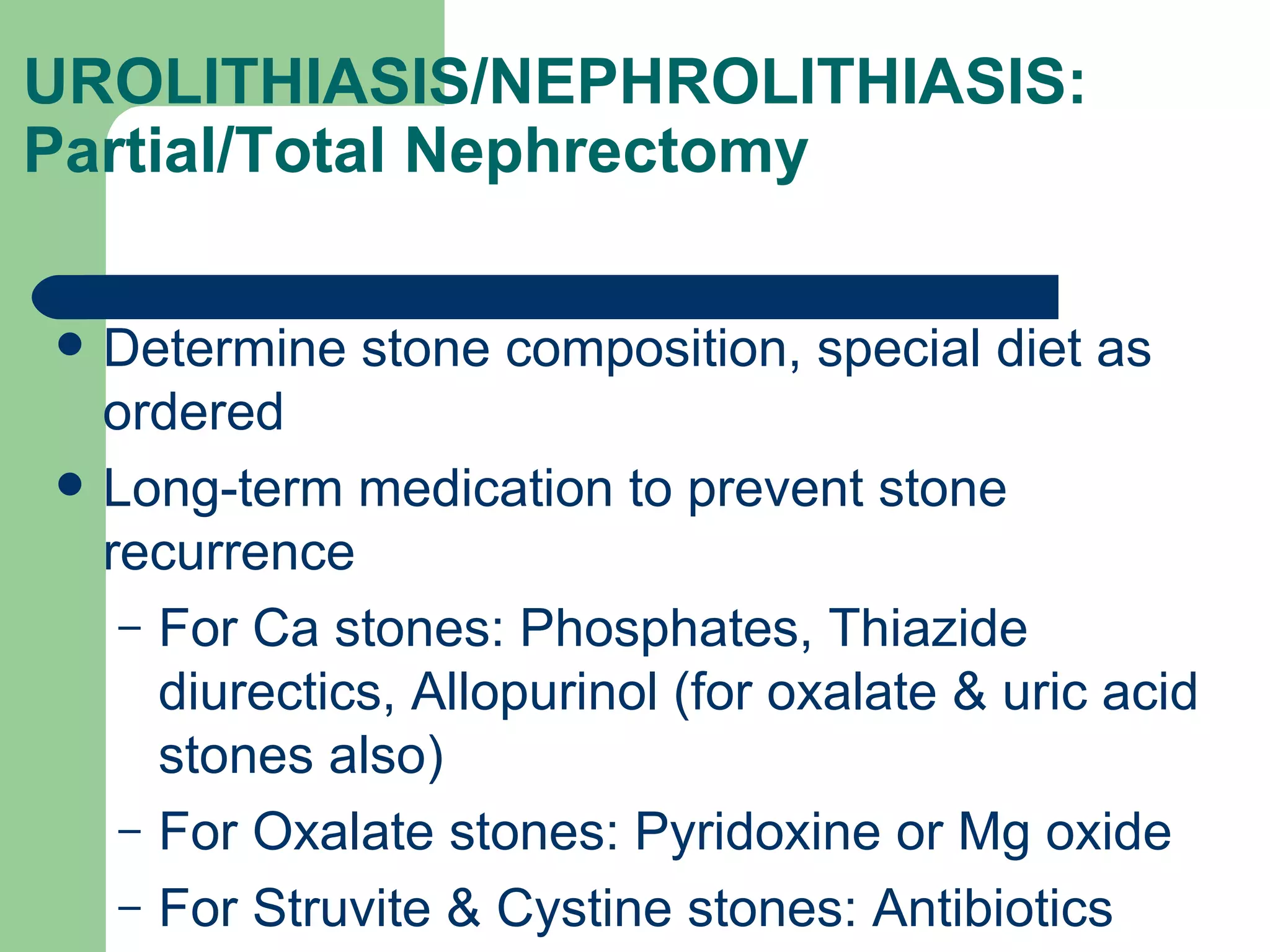
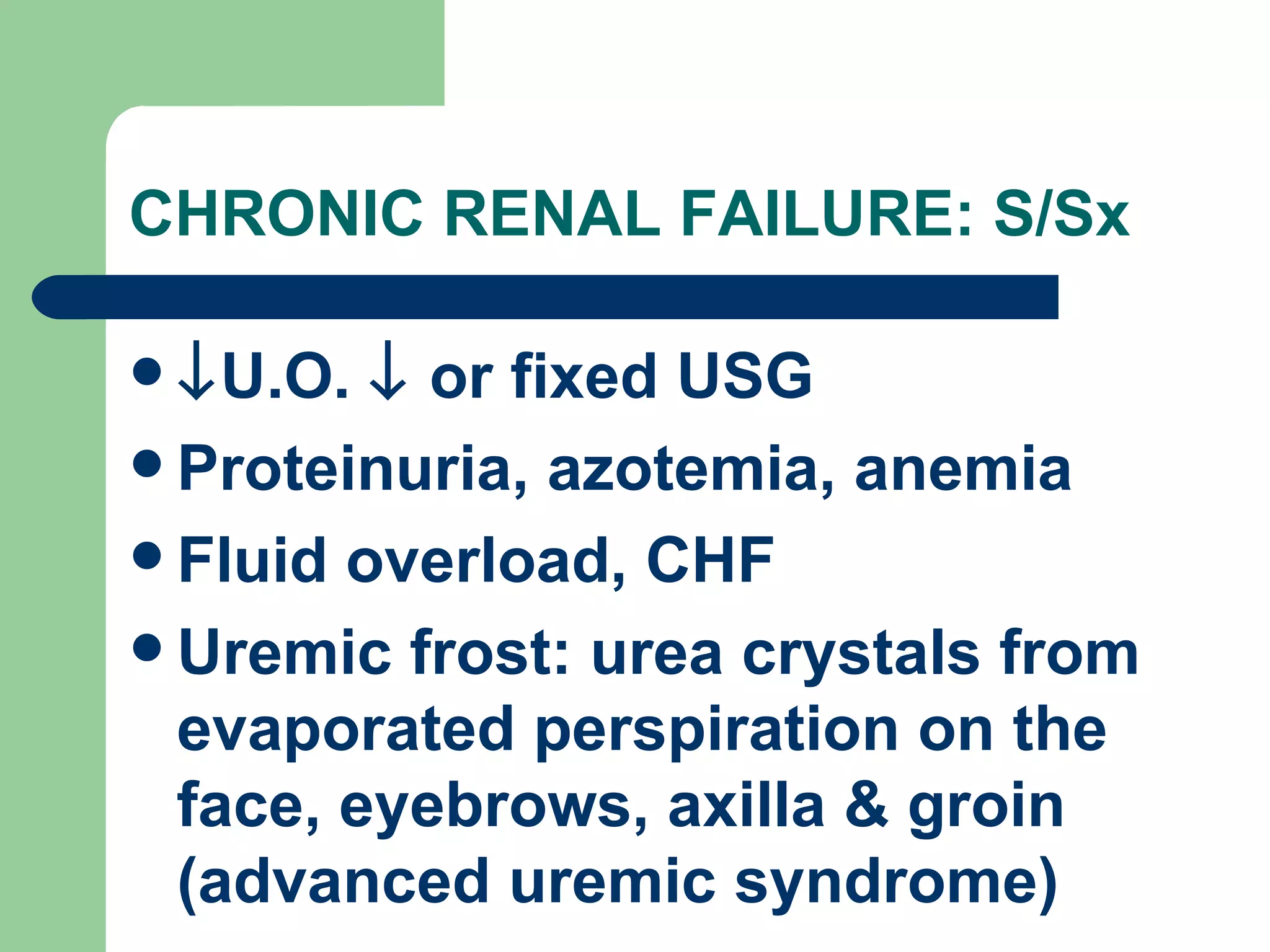
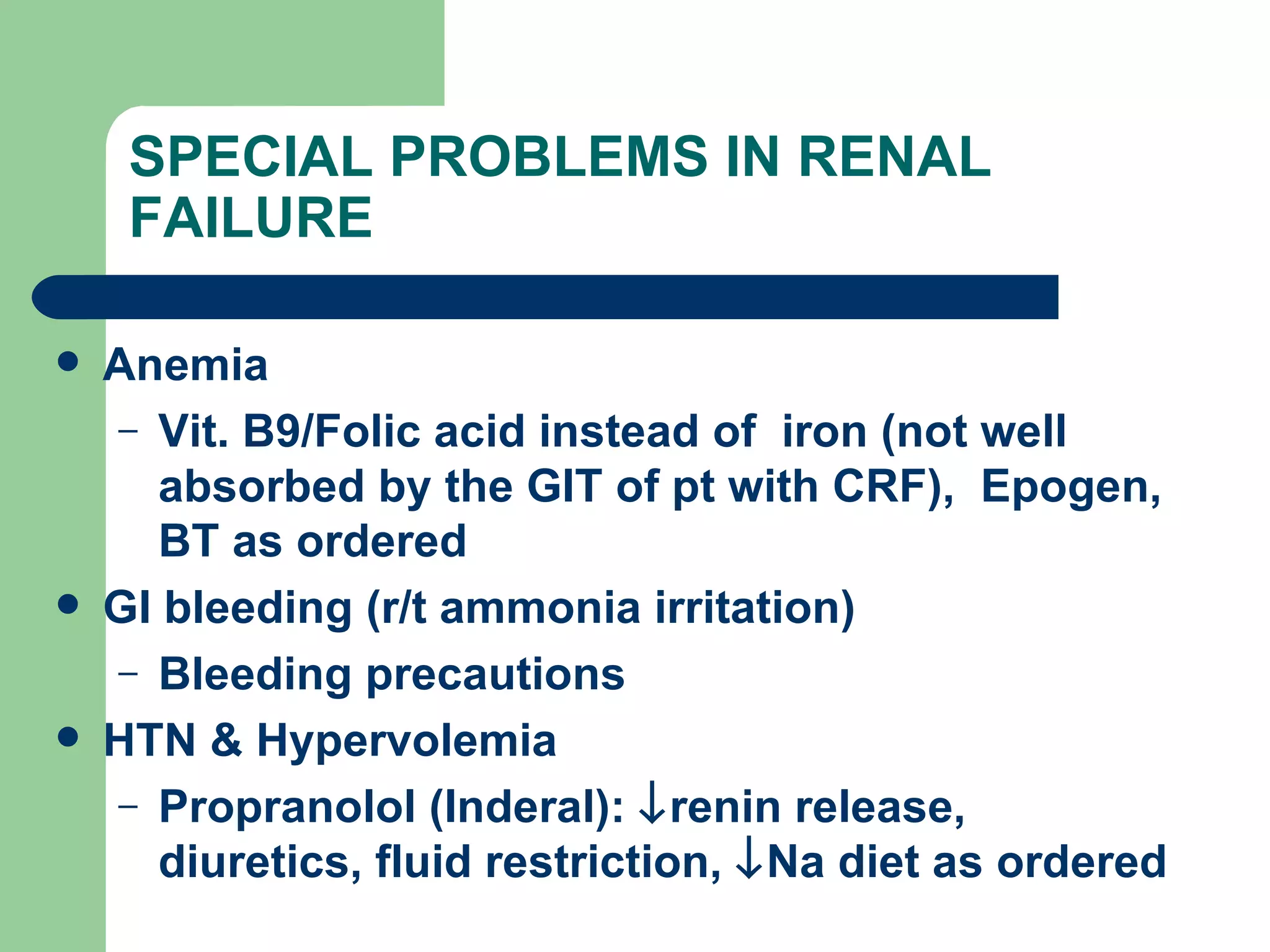
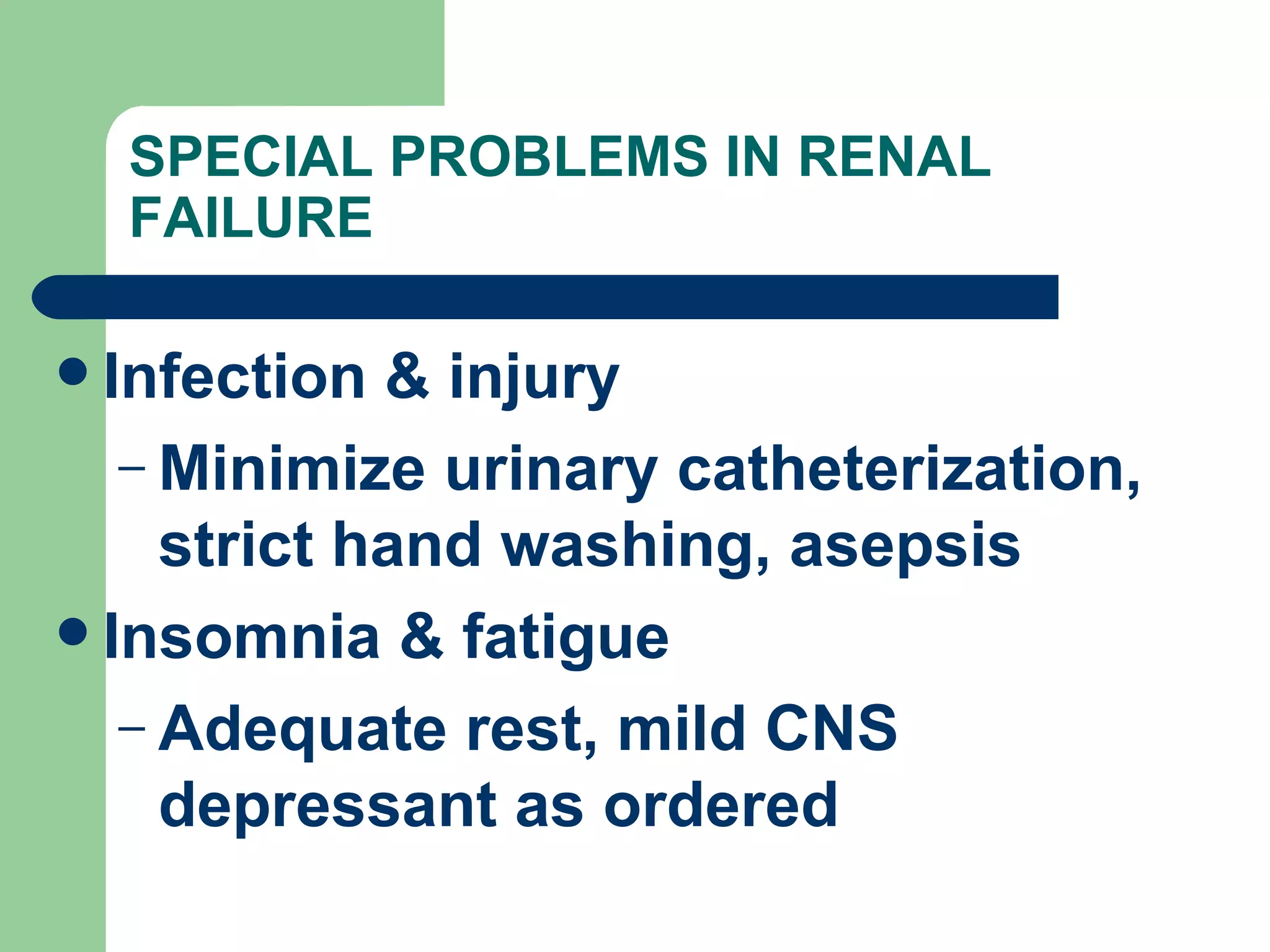
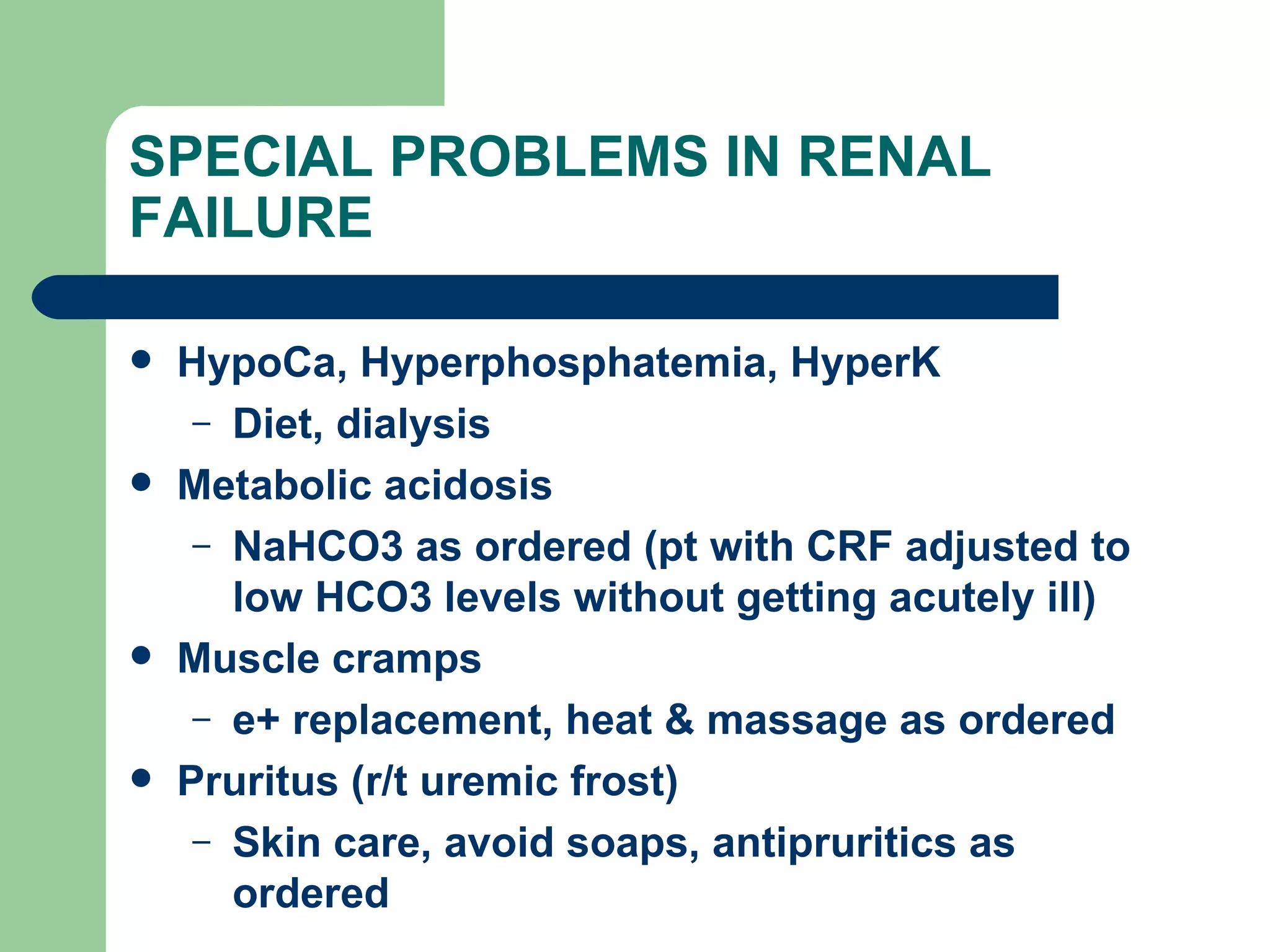
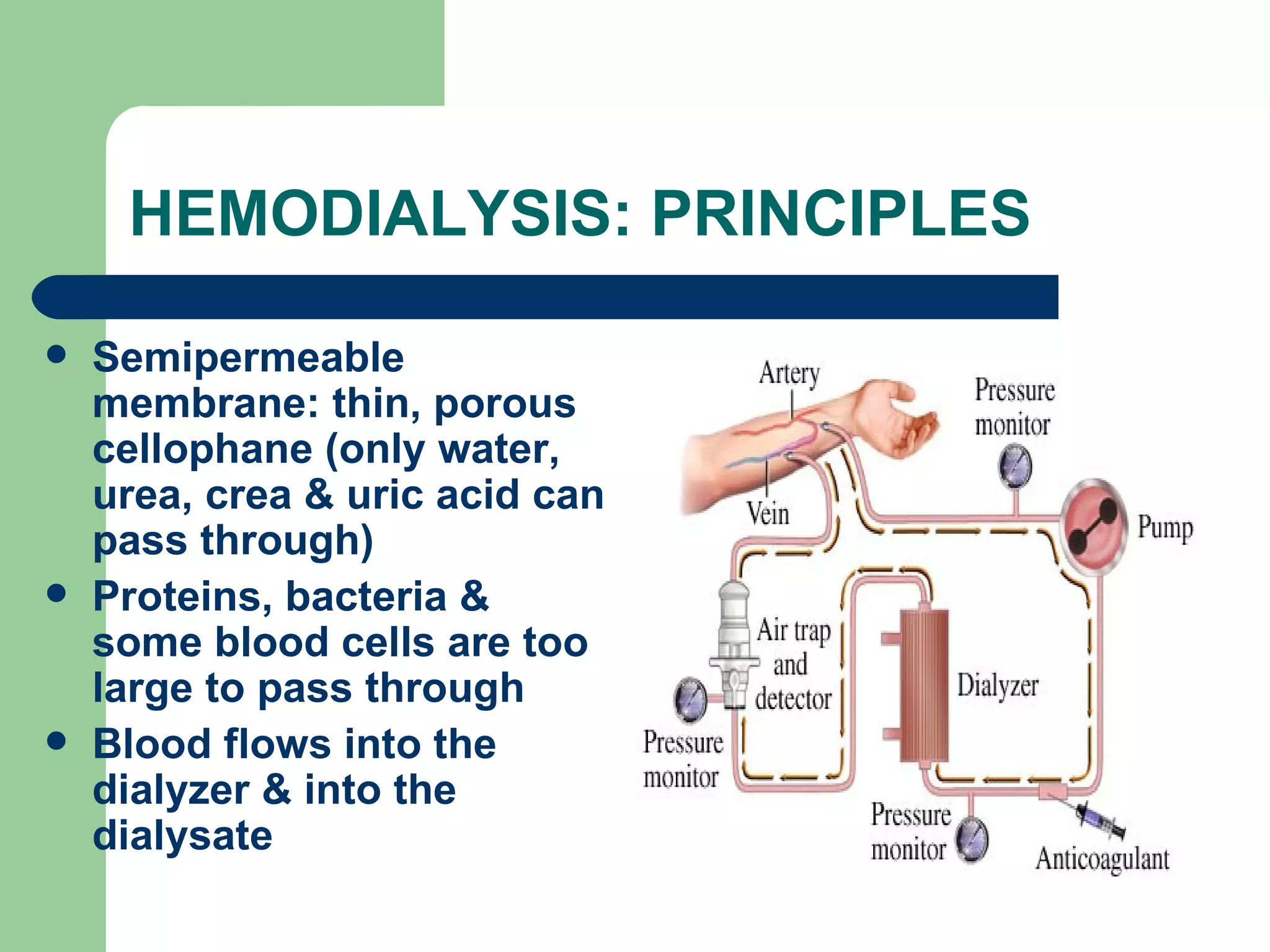
The document provides an overview of the genitourinary system including the kidneys, nephrons, ureters, bladder, prostate gland, and urethra. It discusses common conditions like cystitis, benign prostatic hyperplasia, prostate cancer, urolithiasis, nephrolithiasis, and renal failure. Nursing interventions are outlined for various procedures and post-operative care related to these conditions.