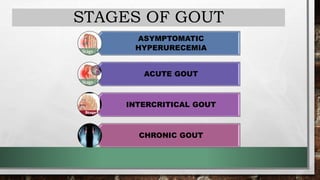
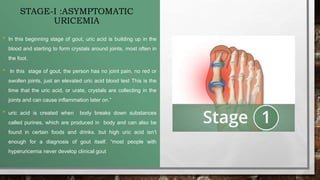
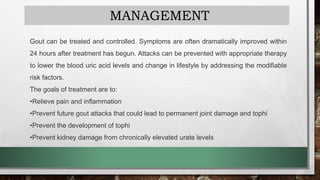
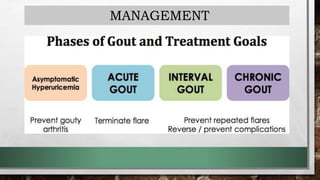
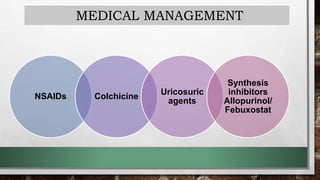
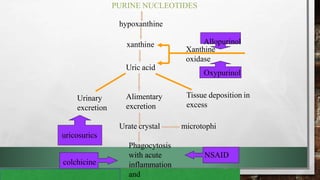
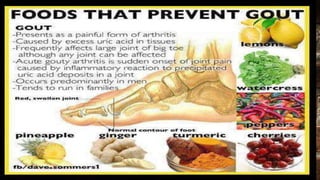
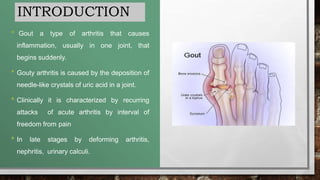
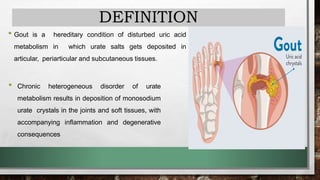
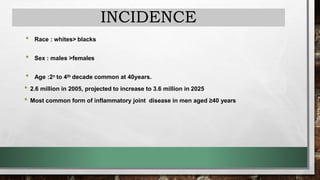
Gout is a type of arthritis caused by high levels of uric acid in the blood. Uric acid crystallizes and deposits in joints, causing sudden, severe attacks of pain, swelling and tenderness. Gout typically affects the big toe joint initially and can progress through stages from asymptomatic hyperuricemia to acute attacks of gouty arthritis, periods of intercritical gout, and finally chronic tophaceous gout if left untreated. Risk factors include genetics, diet high in purines, obesity, medications and other medical conditions.
![ETIOLOGY
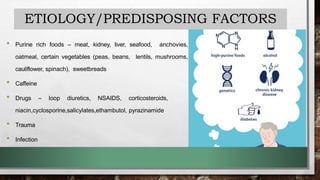
The crystallization of uric acid, often related to relatively high levels in the
blood, is the underlying cause of gout. This can occur because of diet,
genetic predisposition, or underexcretion of urate, the salts of uric acid.[4]
The causes include
• Lifestyle
• Genetics
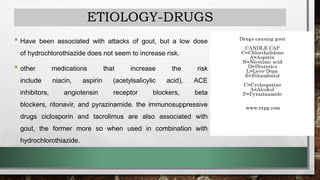
• Drugs
• Medical conditions](https://image.slidesharecdn.com/goutyarthritis-200720103928/85/Gouty-arthritis-7-320.jpg)