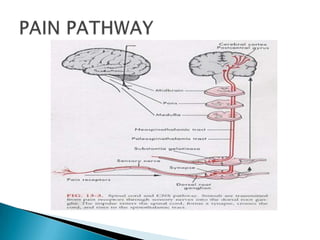
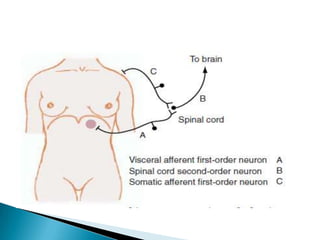
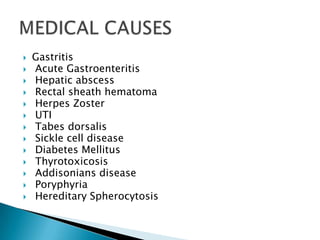
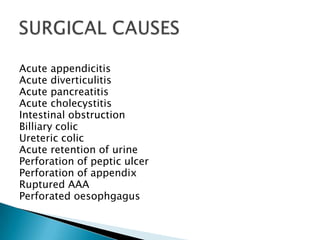
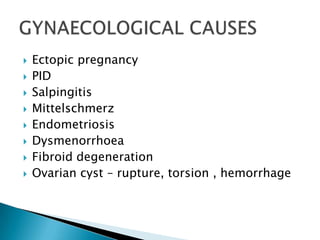
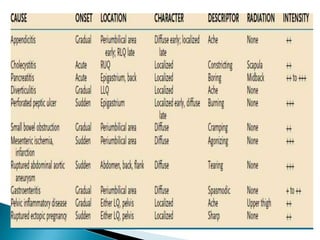
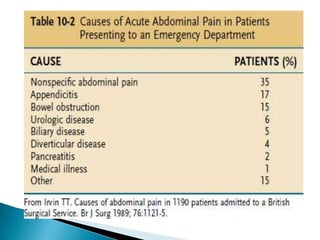
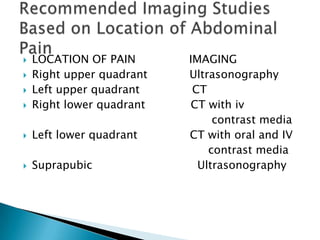
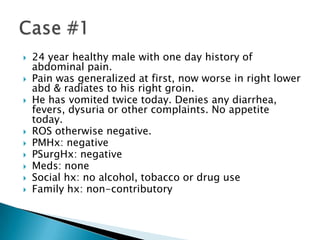
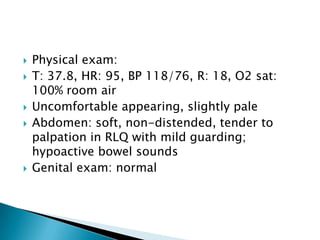
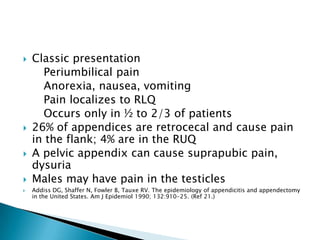
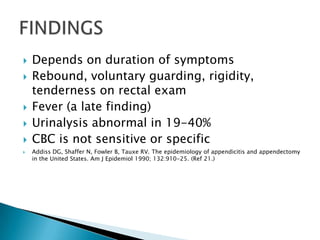
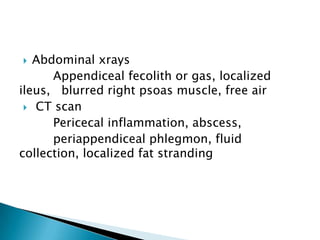
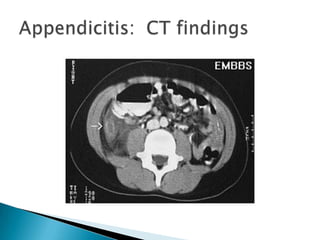
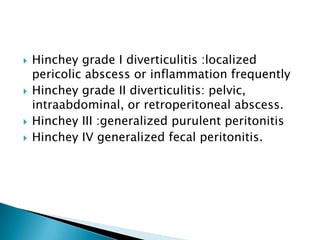
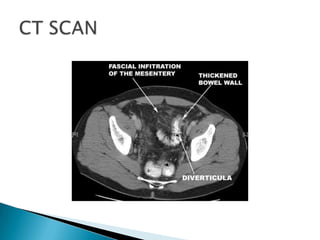
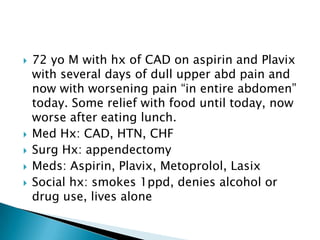
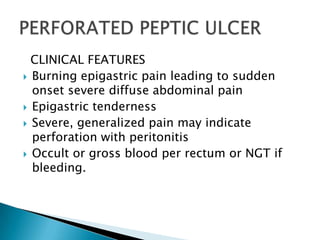
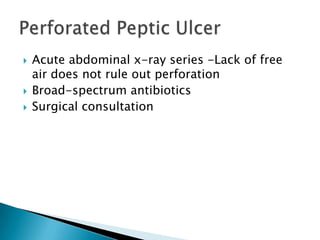
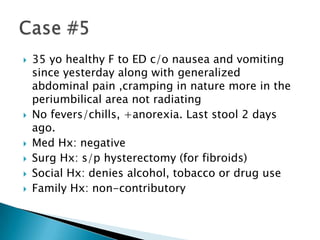
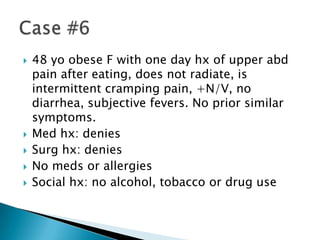
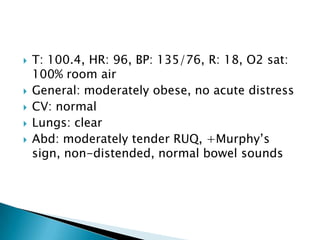
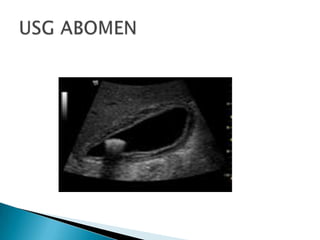
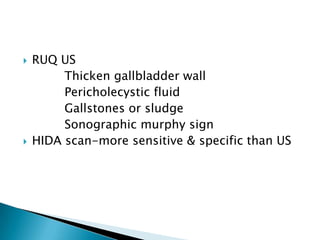
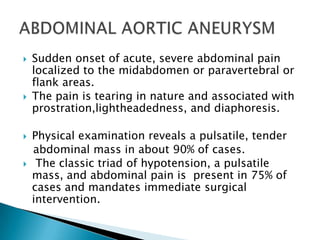
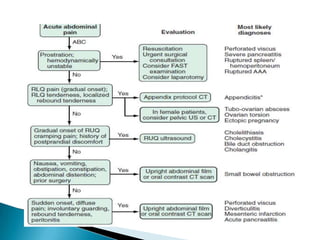
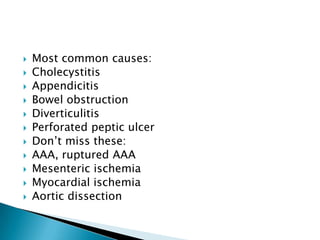
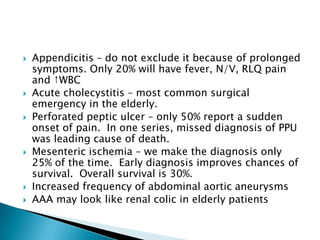
This document provides an overview of abdominal pain. It defines three types of pain: visceral, parietal, and referred. Visceral pain is poorly localized and involves hollow organs. Parietal pain is sharp and well-localized. Referred pain is felt remotely from the site of injury. Common causes of abdominal pain and their clinical features are described. Evaluation may involve imaging like ultrasound or CT scan depending on location of pain. Management is discussed for specific conditions like appendicitis, diverticulitis, and pancreatitis. Surgical consultation and antibiotics are often involved in treatment.