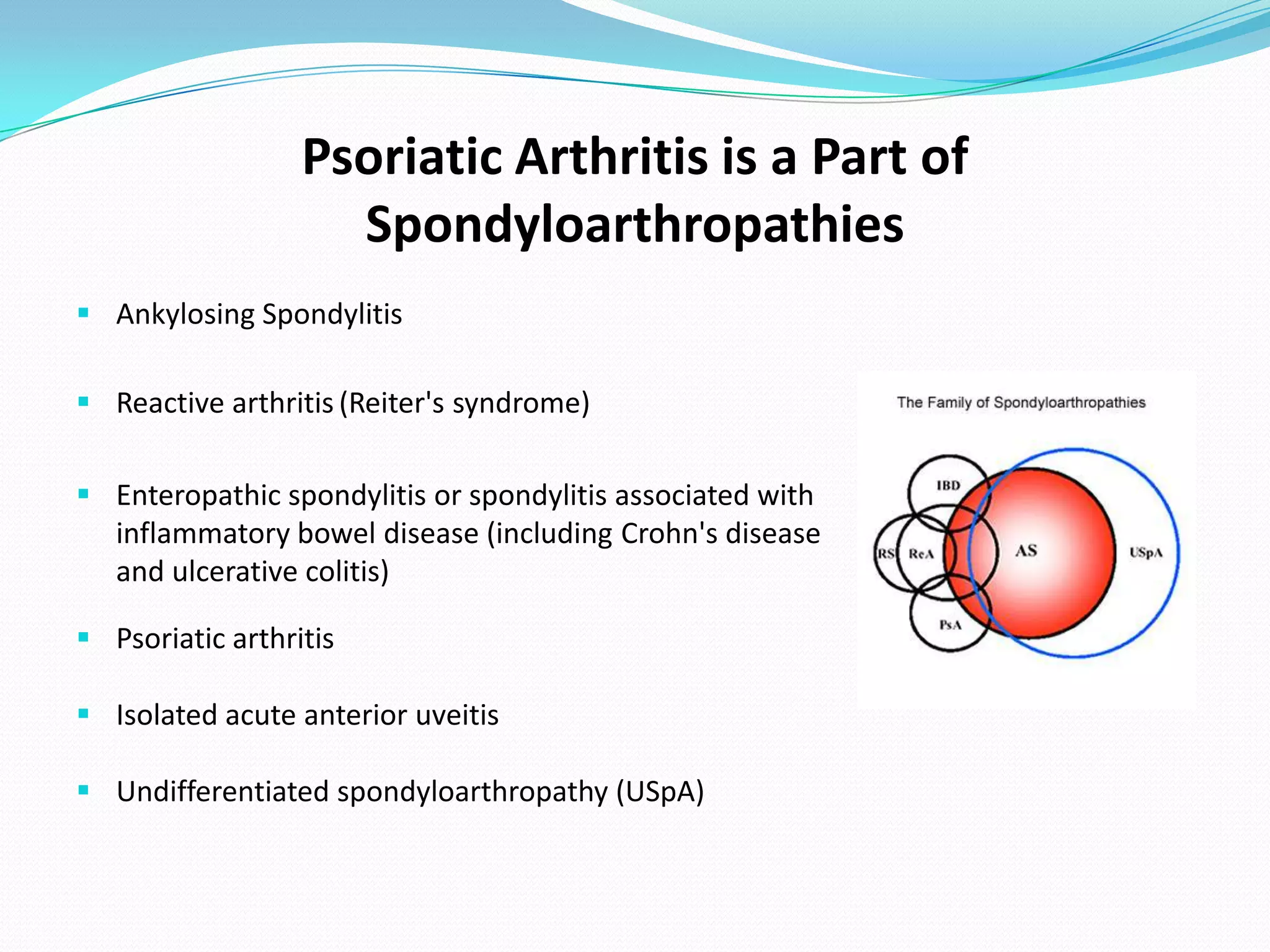
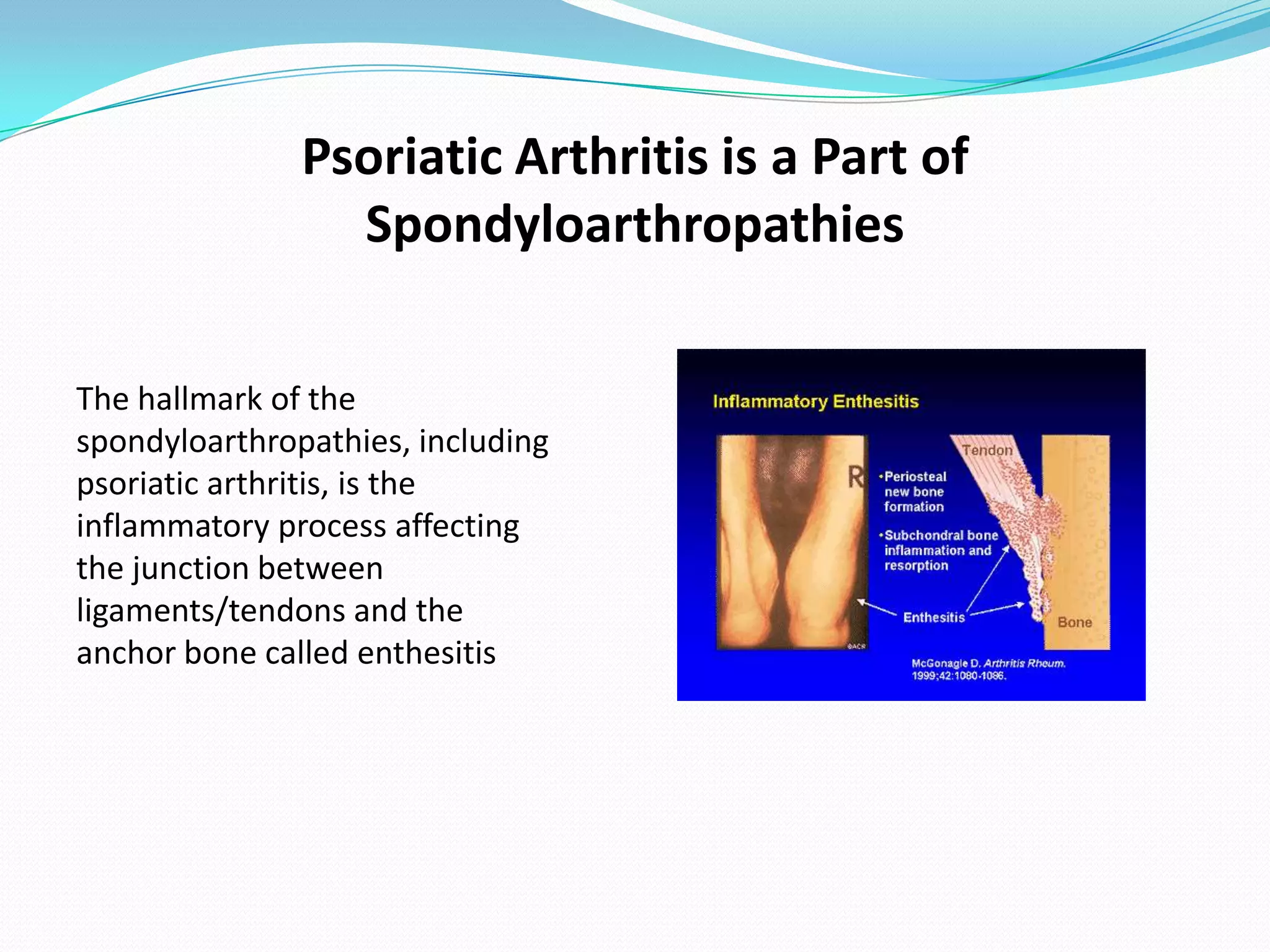
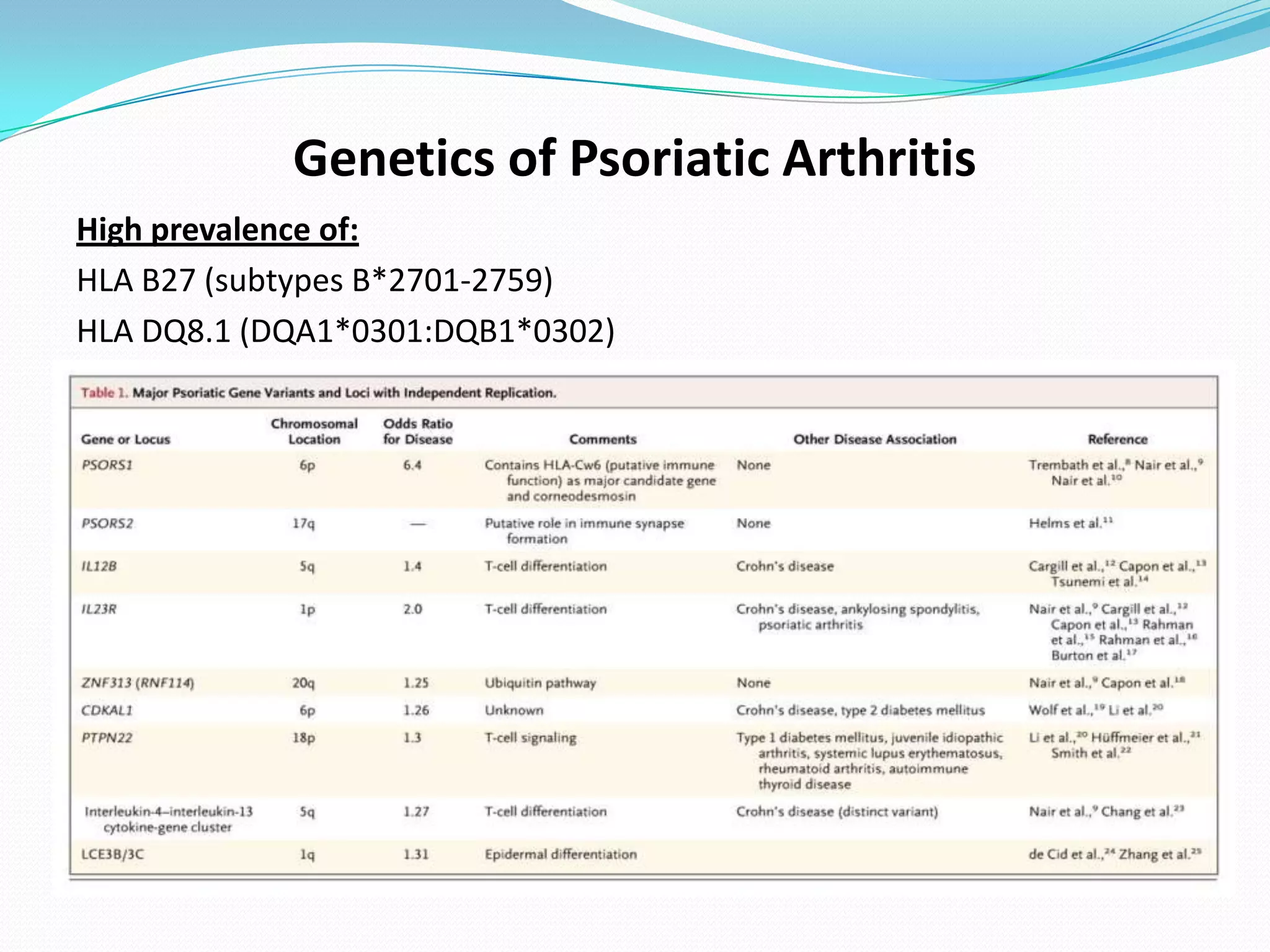
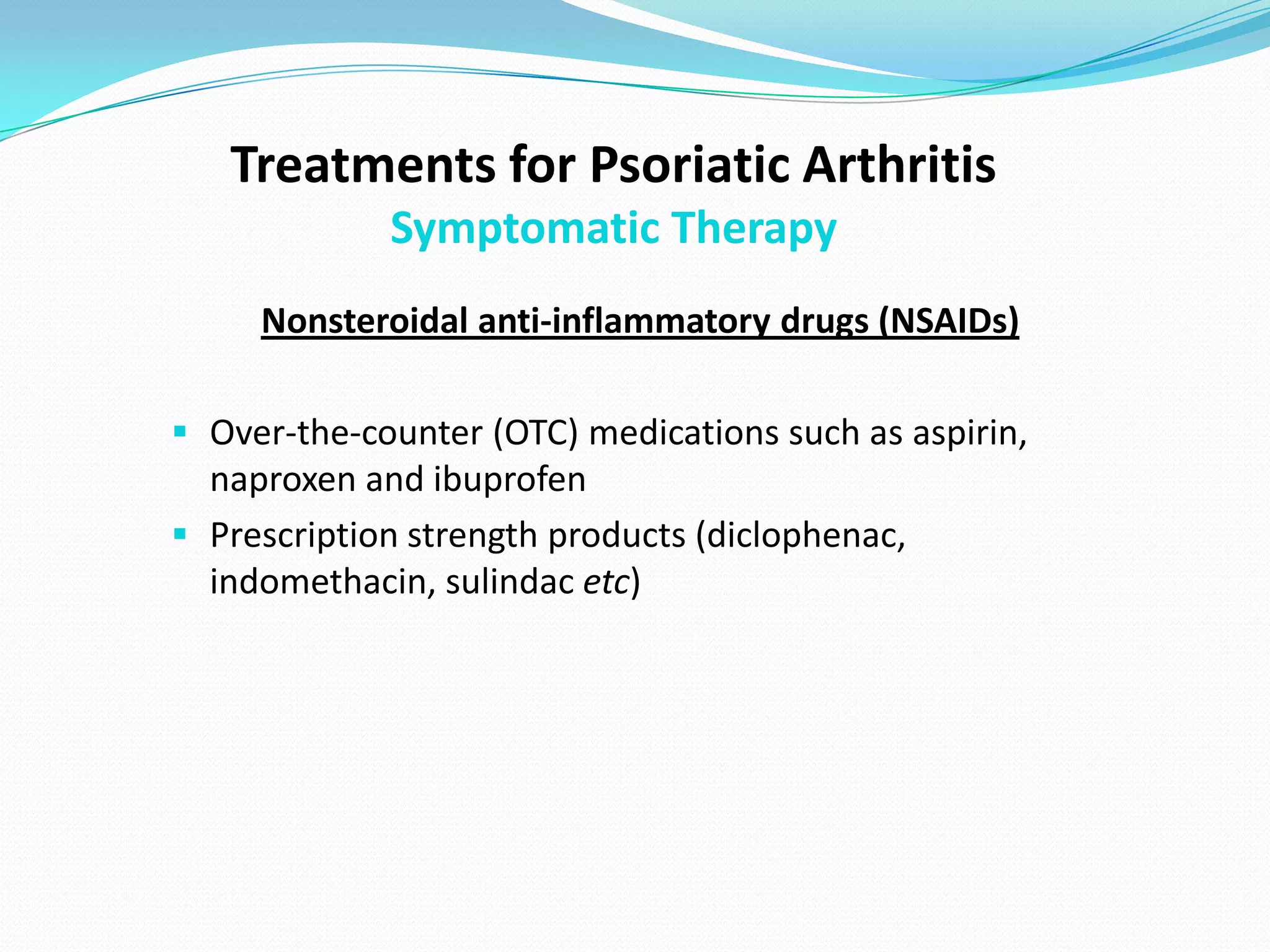
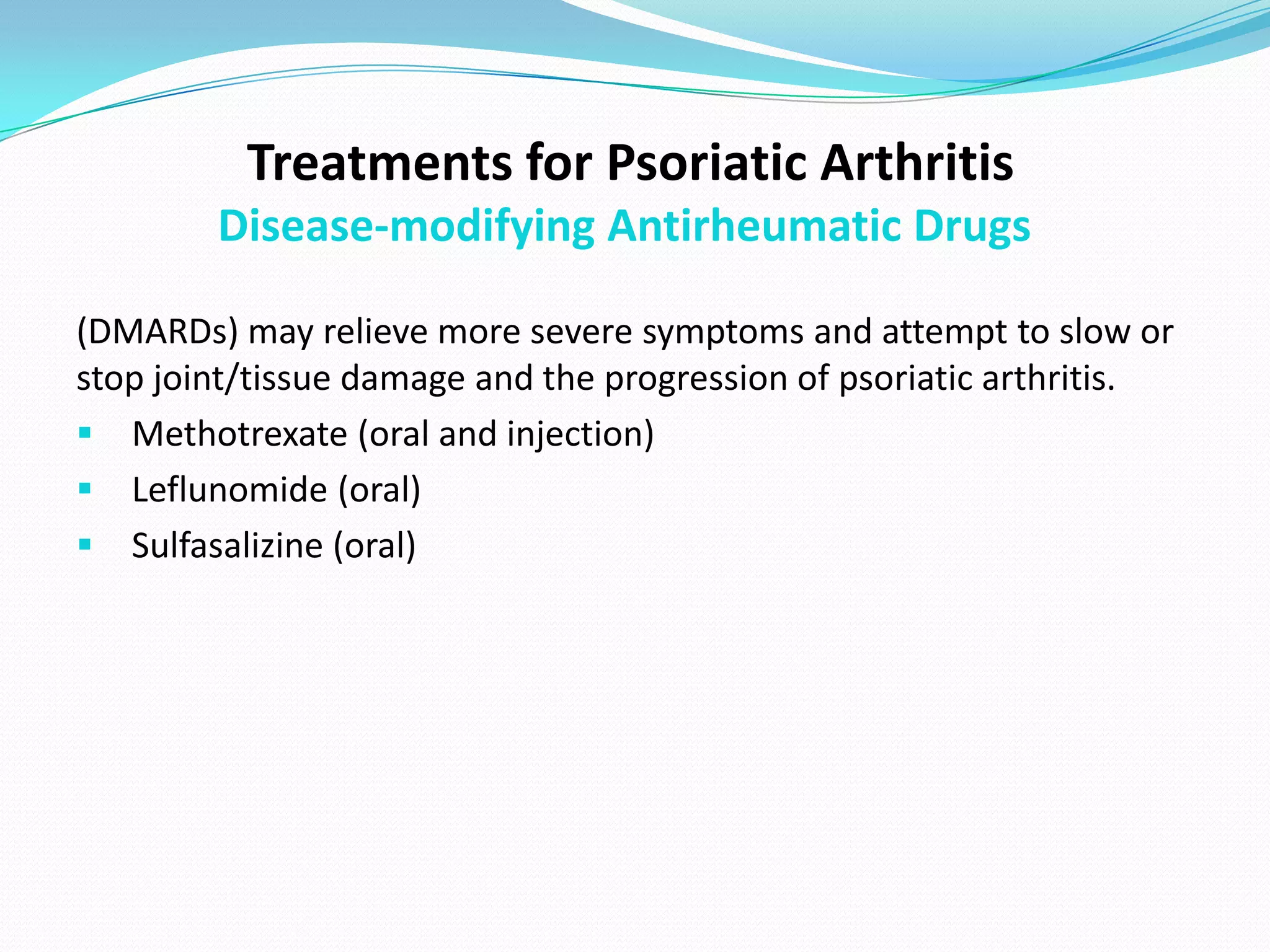
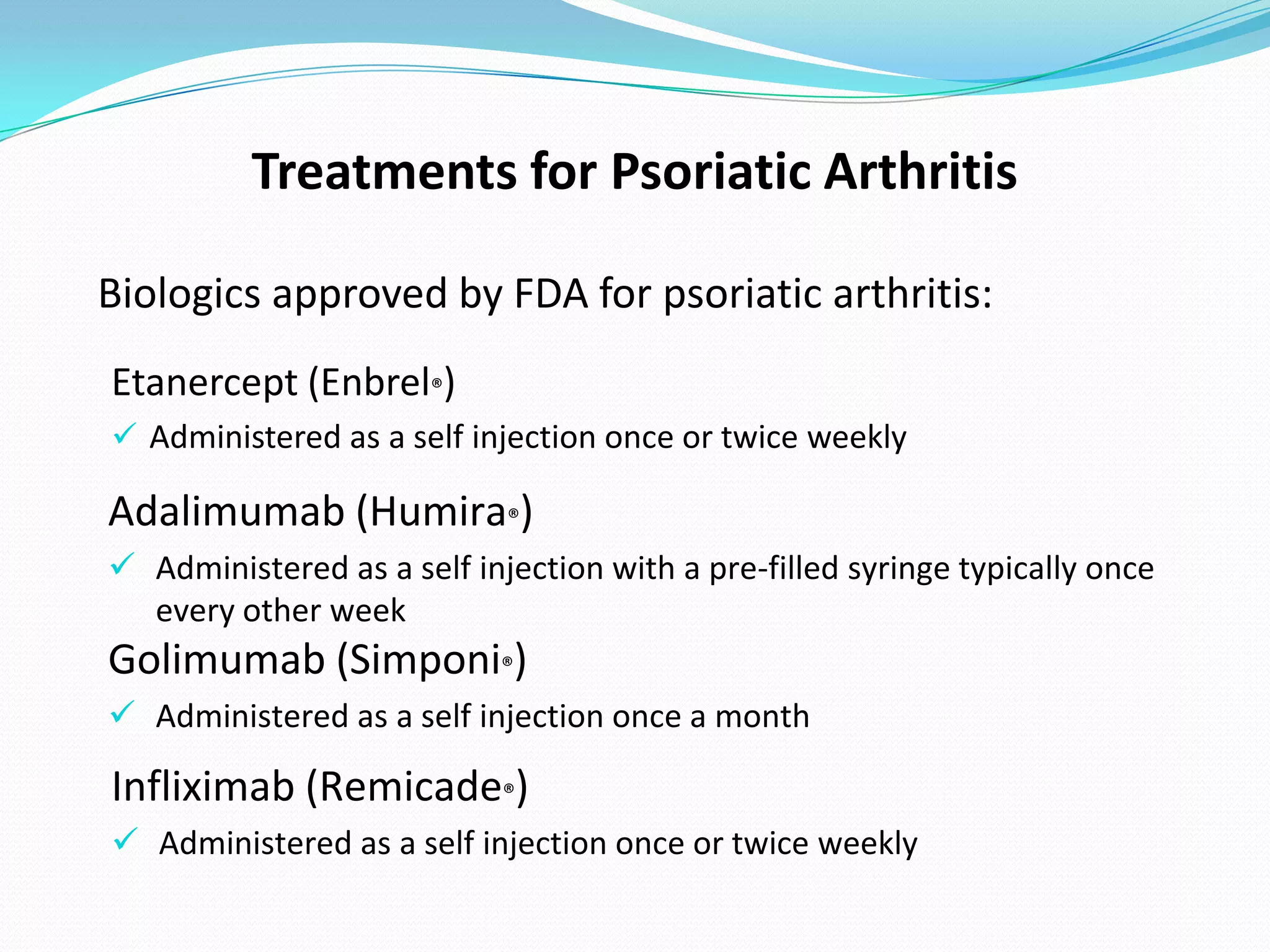
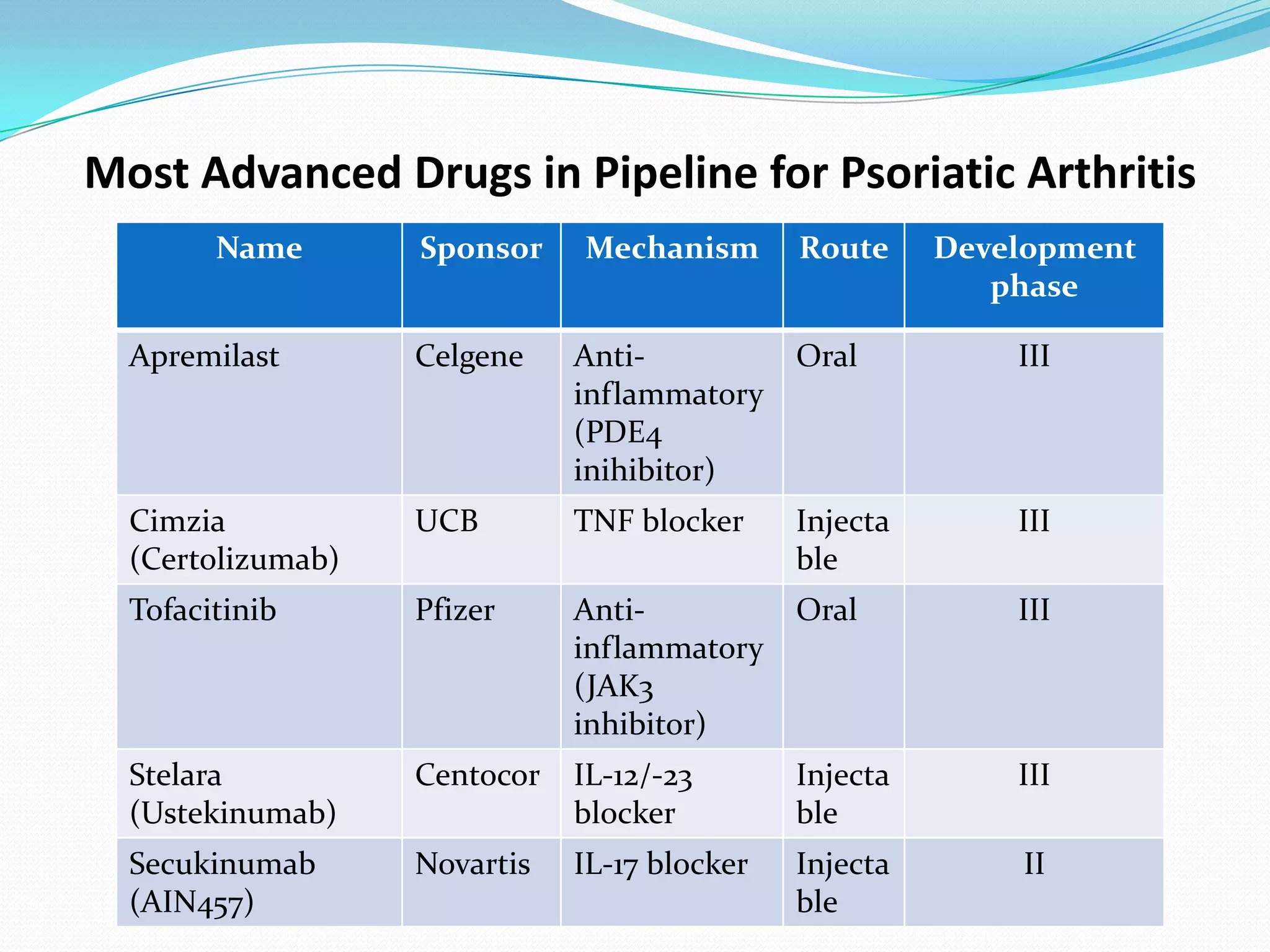
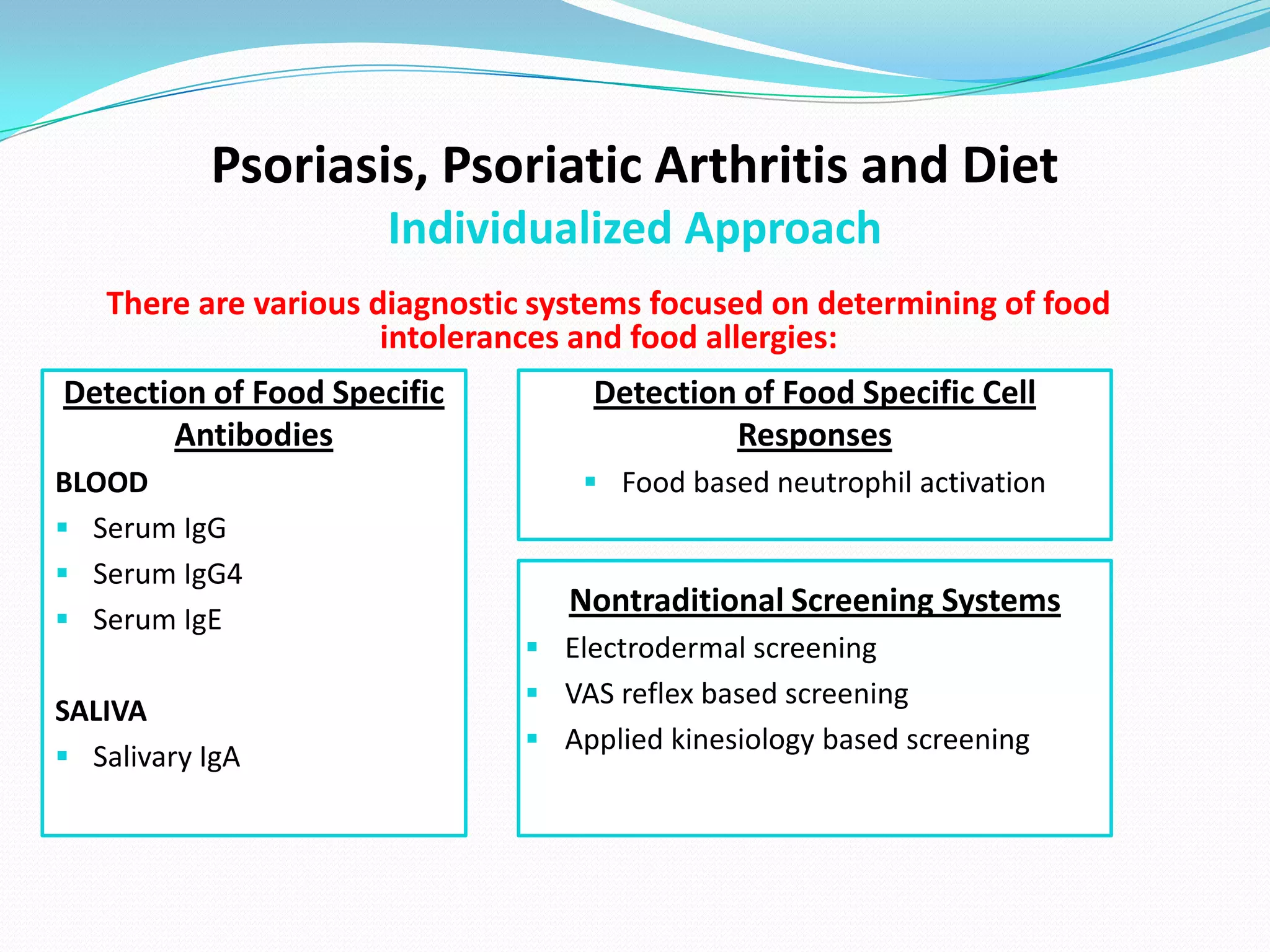
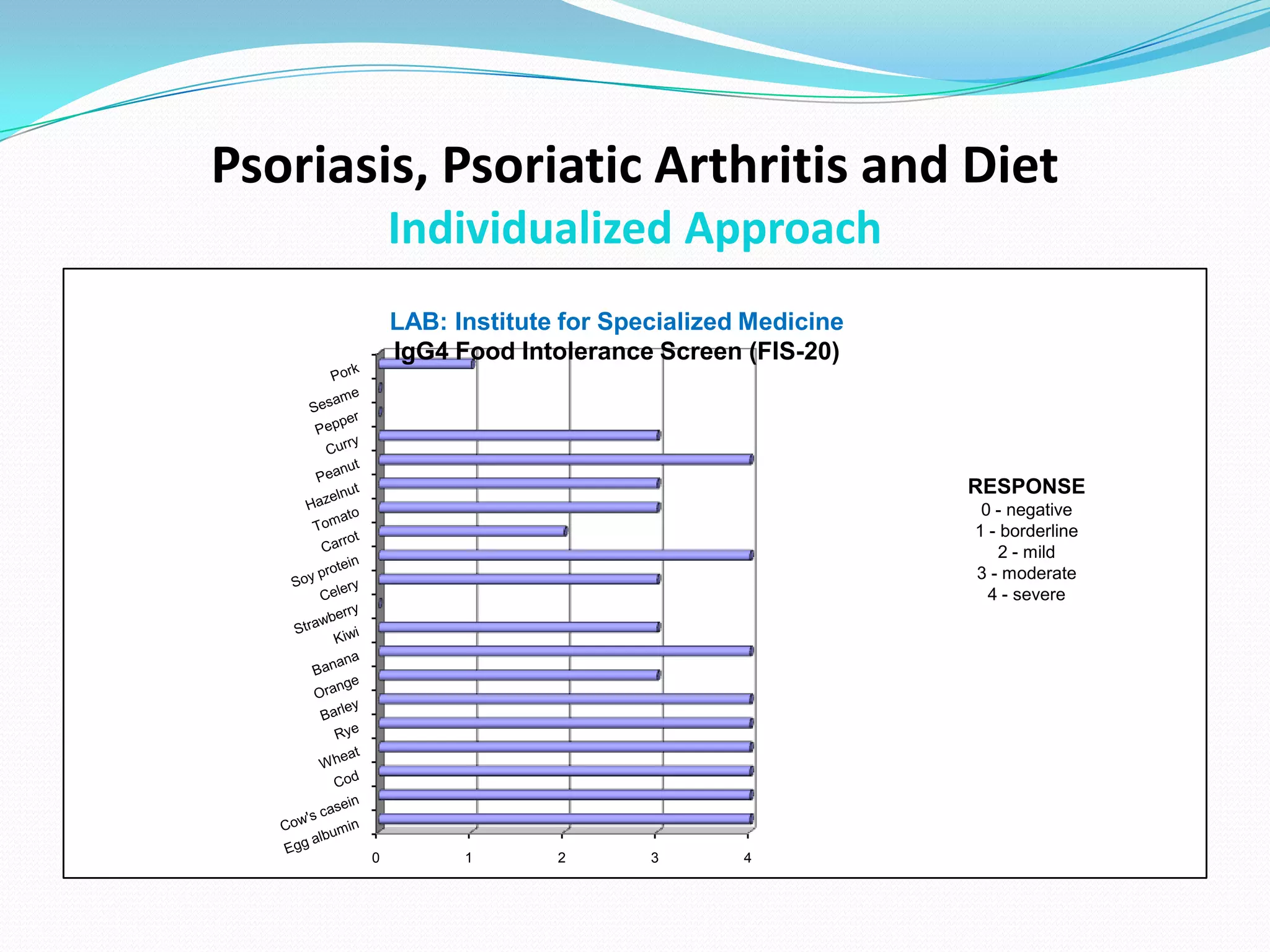
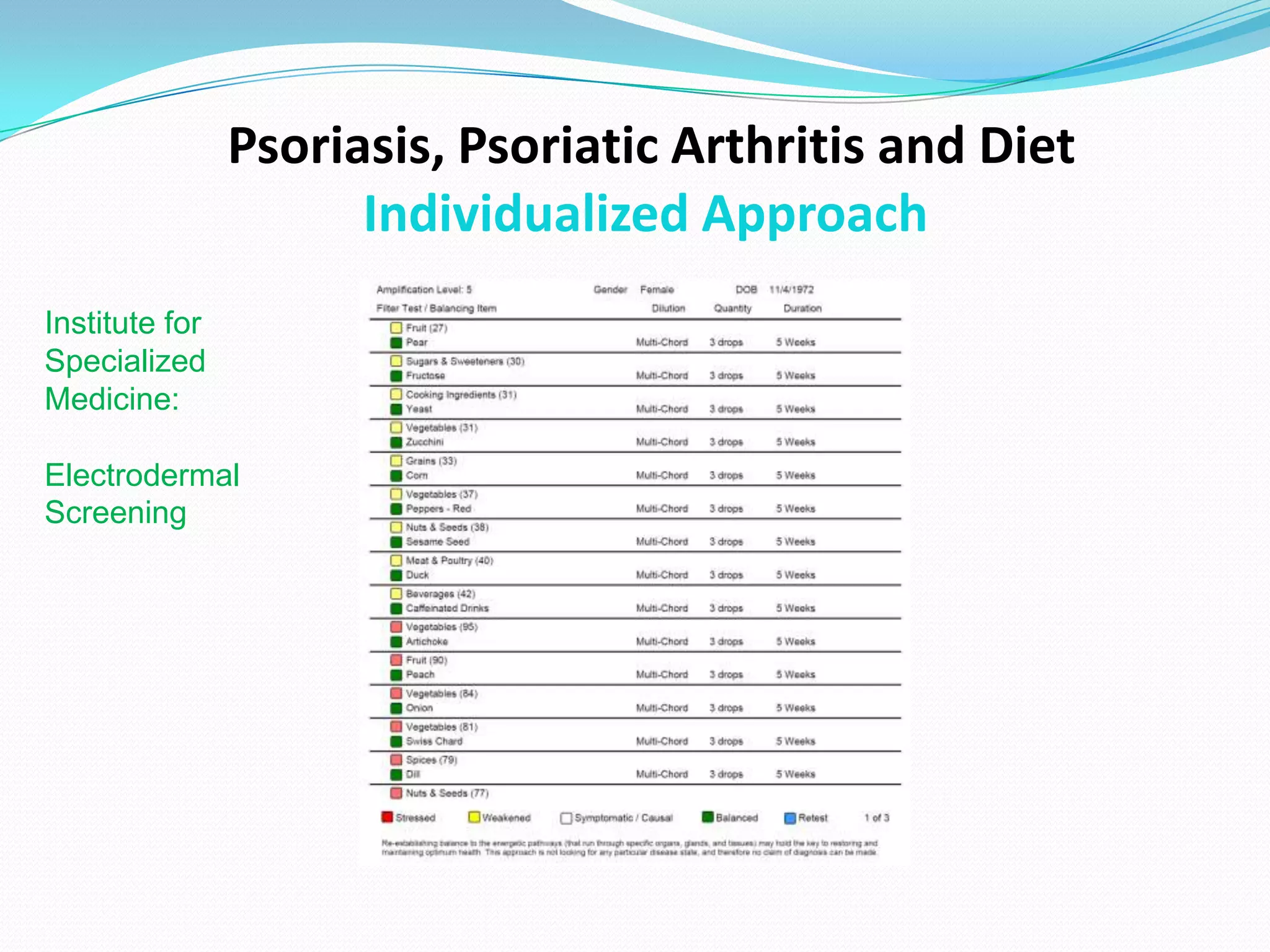
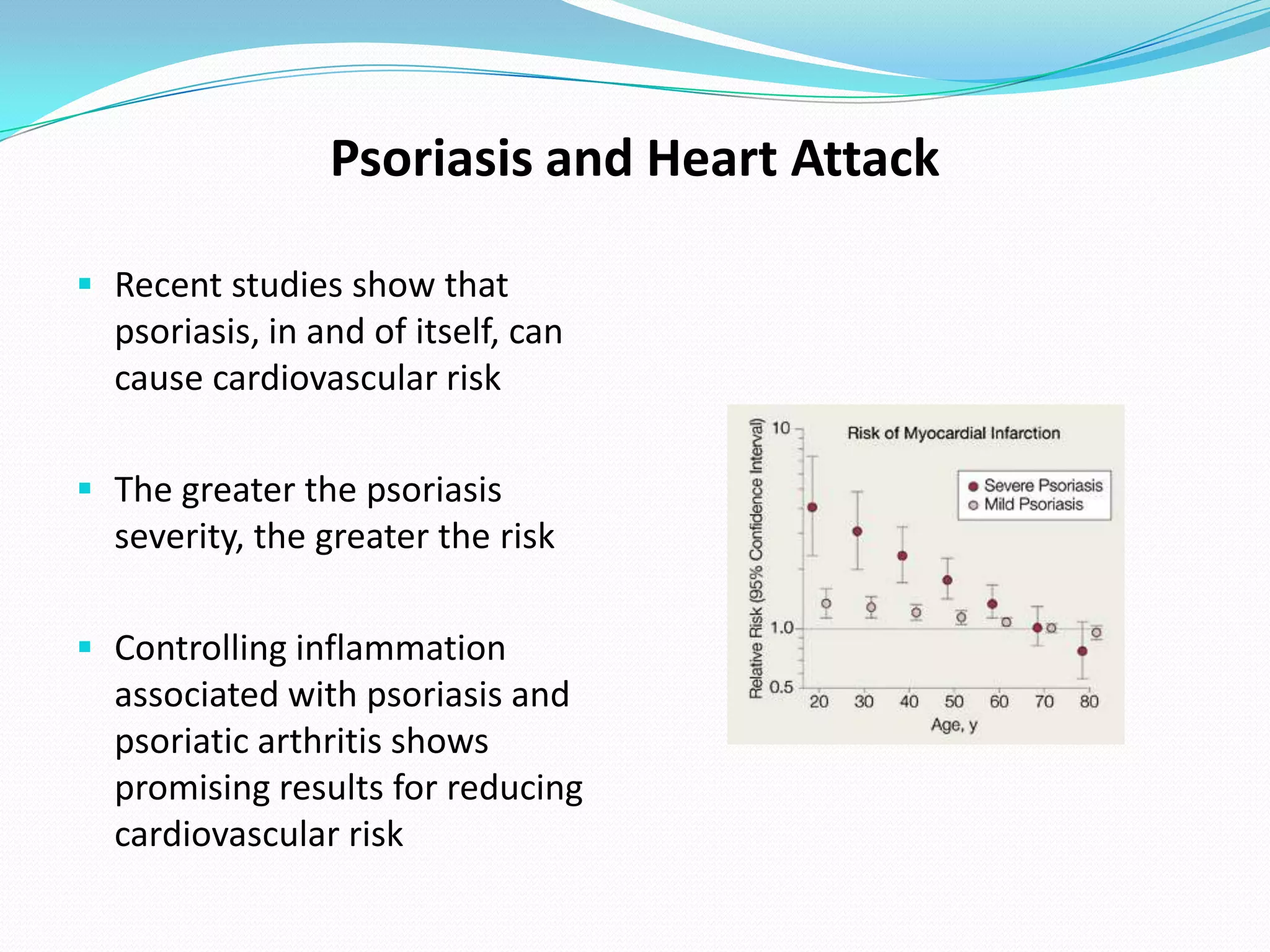
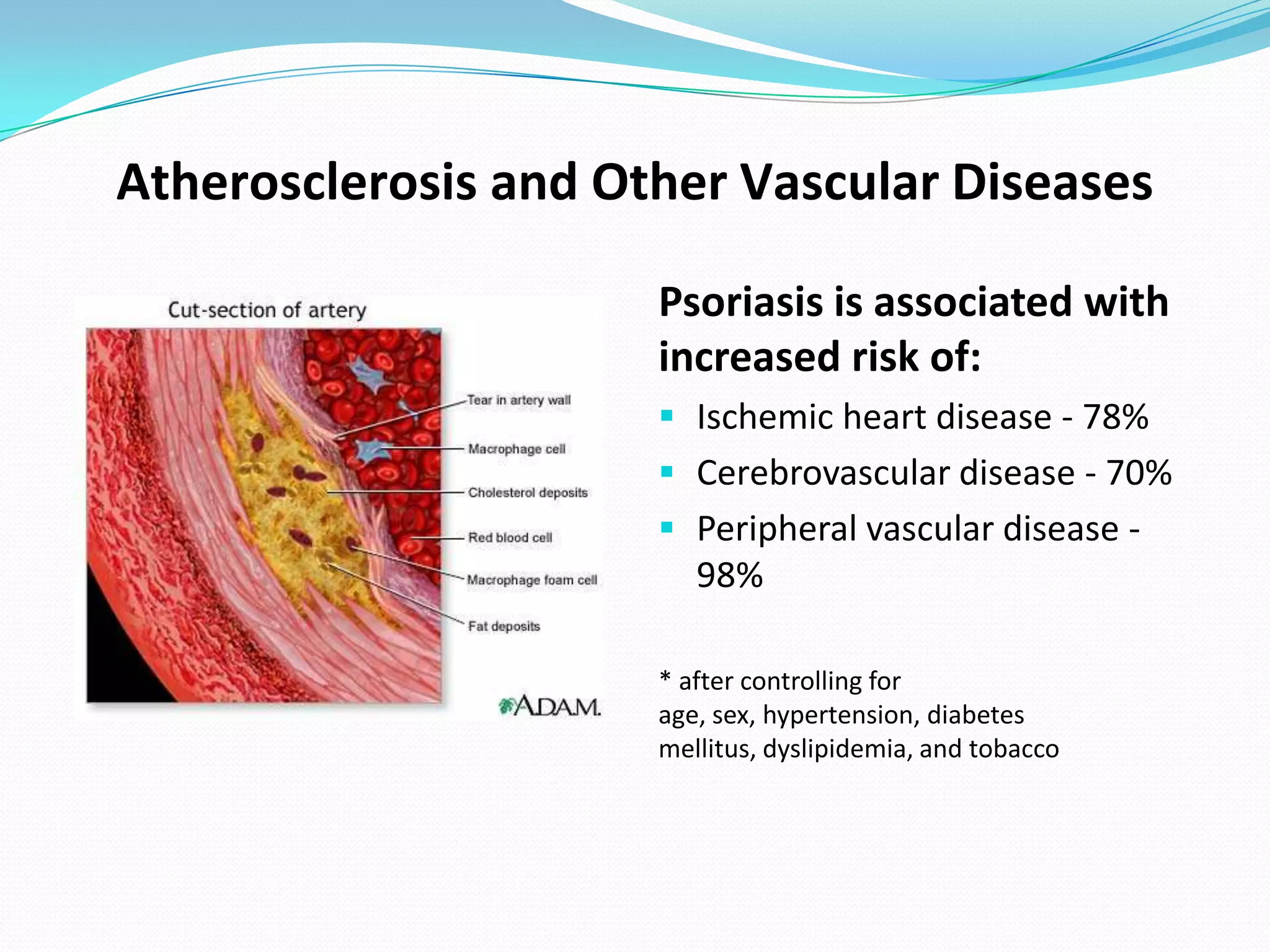
This document discusses psoriatic arthritis, including its causes, symptoms, diagnosis, subtypes, and treatment options. It notes that psoriatic arthritis affects up to 30% of people with psoriasis, causing joint pain, stiffness and swelling. Both non-steroidal anti-inflammatory drugs and disease-modifying drugs can help treat symptoms, while biologics approved for psoriatic arthritis include etanercept, adalimumab, golimumab and infliximab. Diet and food sensitivities also play a role, so an individualized approach considering food intolerance testing and elimination diets is recommended.