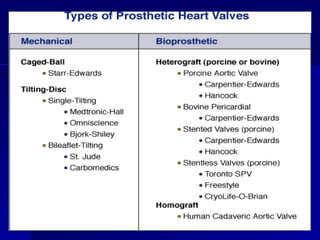
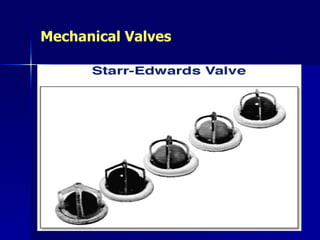
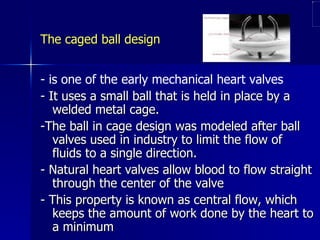
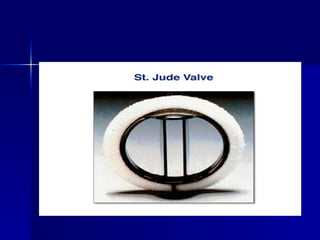
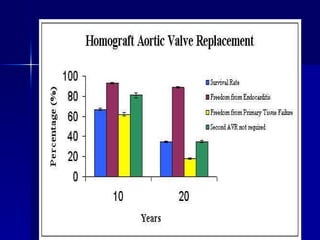
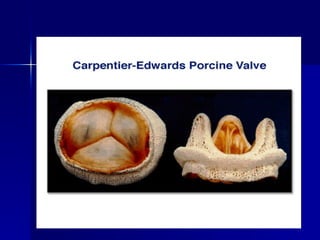
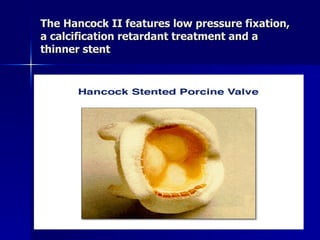
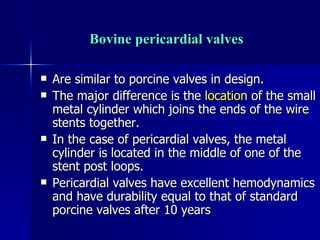
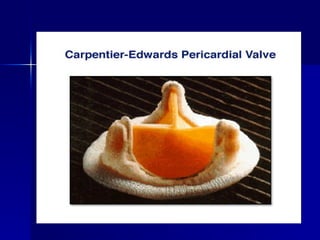
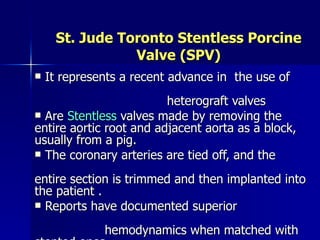
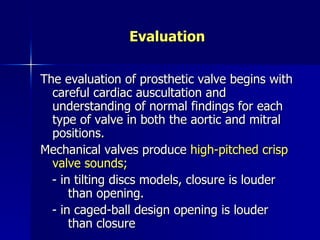
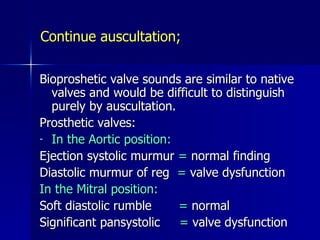
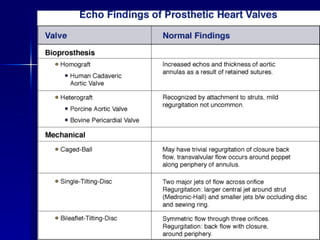
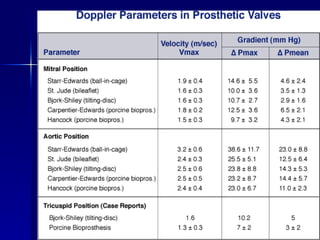
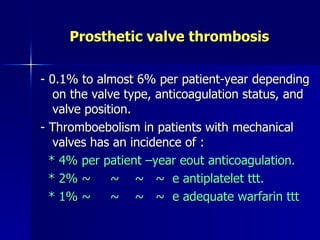
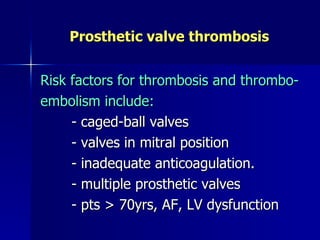
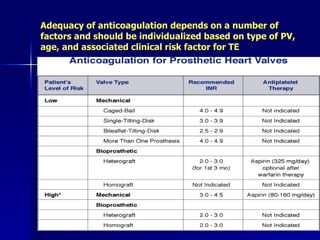
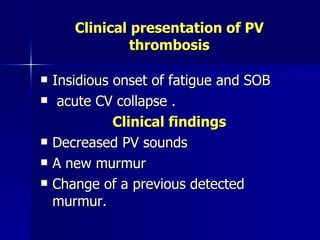
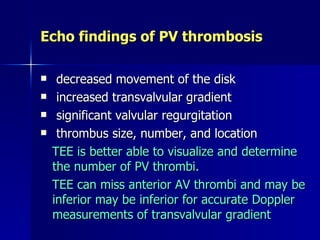
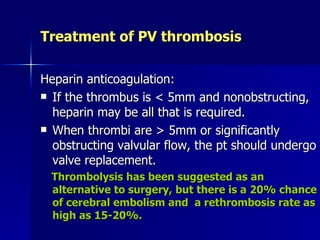
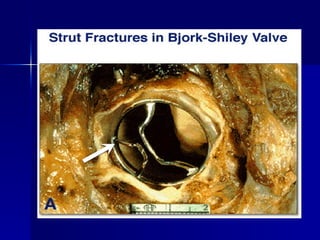
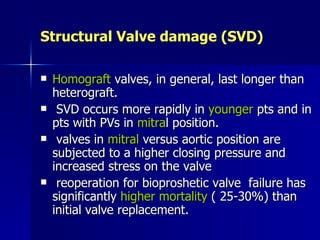
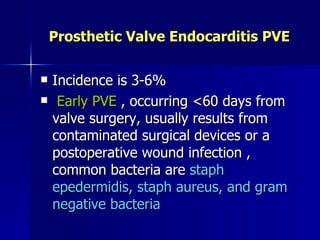
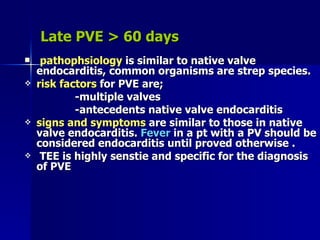
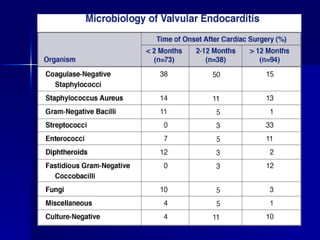
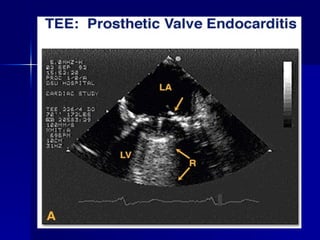
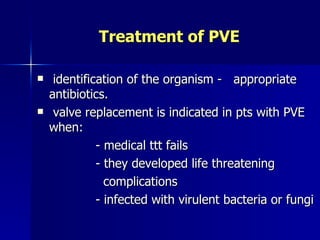
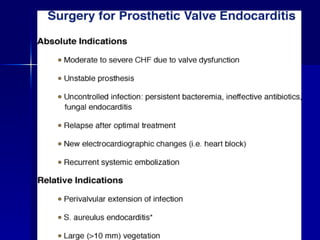
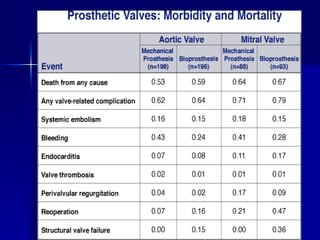
Mechanical and bioprosthetic heart valves have evolved significantly since the first prosthetic valve implantation in 1952. Modern bileaflet mechanical valves provide improved central blood flow compared to older caged ball designs. Tissue valves like porcine and pericardial valves do not require lifelong anticoagulation but have limited durability. Prosthetic heart valves are prone to complications like thrombosis, structural deterioration, endocarditis, and paravalvular leak. Careful monitoring and treatment is needed to optimize outcomes.