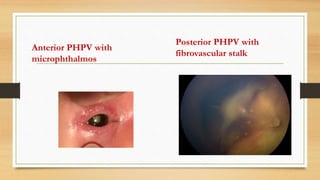
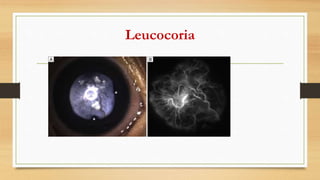
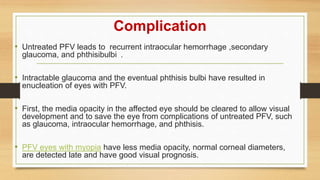
This document provides information on persistent hyperplastic primary vitreous (PHPV), a congenital eye disorder caused by the failure of the embryonic primary vitreous and blood vessels to regress. It describes the classification, history, clinical features, diagnosis, complications, and management of both anterior and posterior PHPV. Anterior PHPV involves remnants attached to the back of the lens, while posterior PHPV involves remnants arising from the optic nerve; posterior PHPV tends to be more destructive. Treatment may involve surgery such as lensectomy with vitrectomy to clear media opacity and prevent complications like glaucoma.