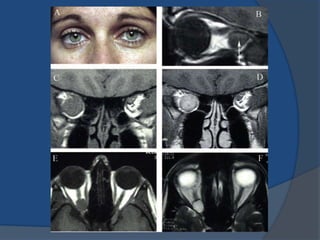
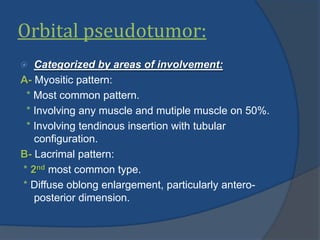
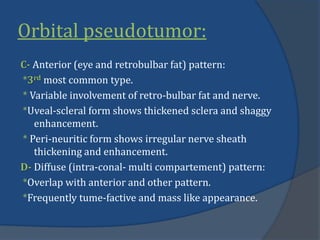
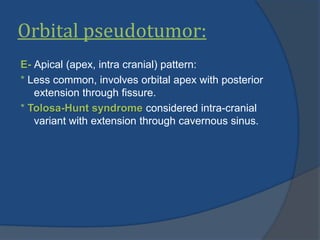
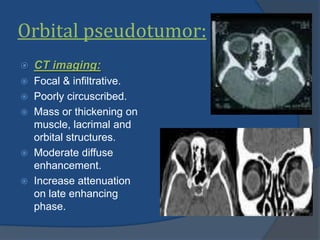
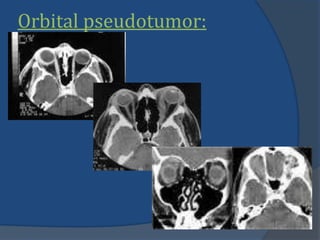
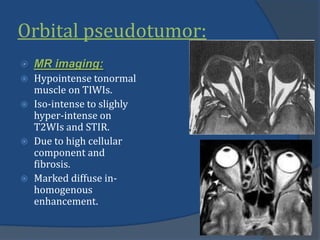
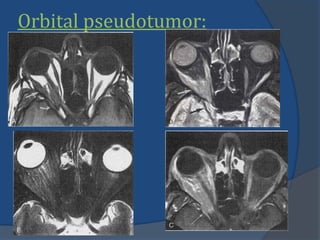
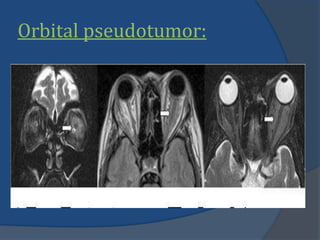
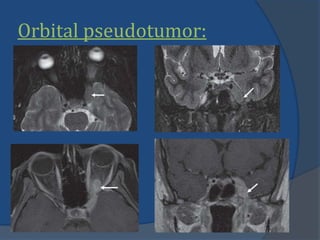
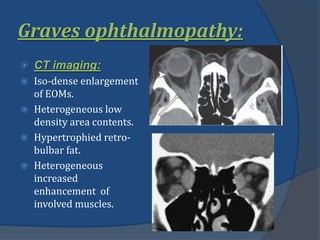
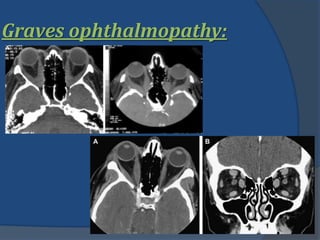
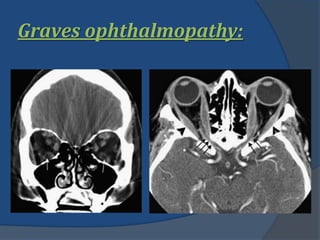
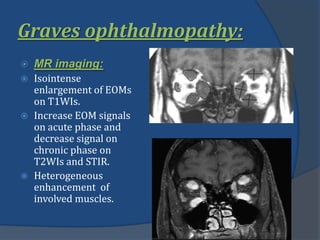
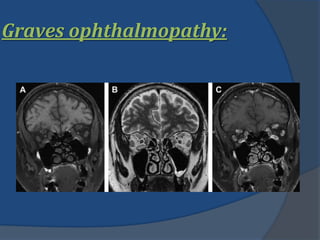
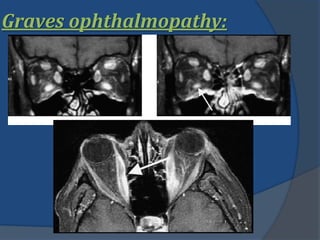
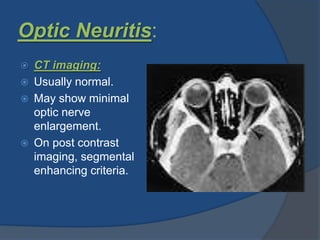
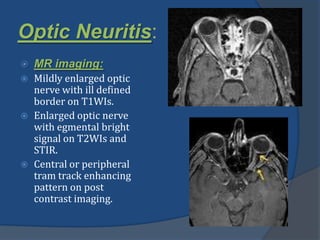
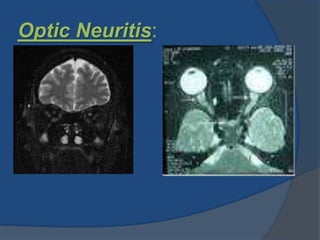
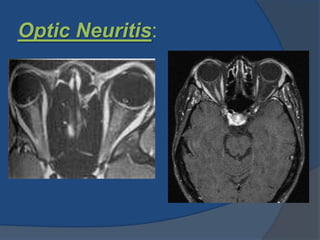
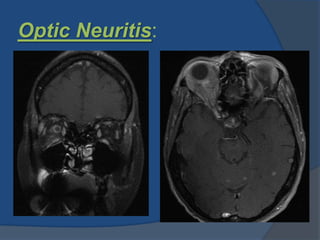
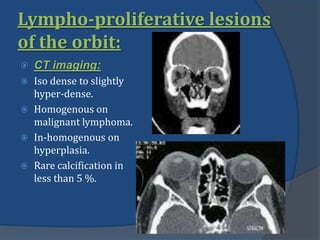
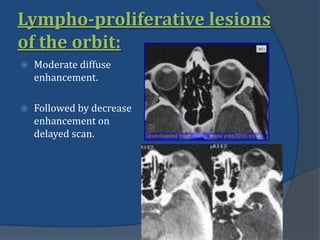
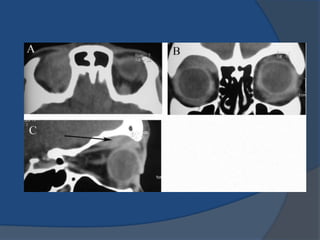
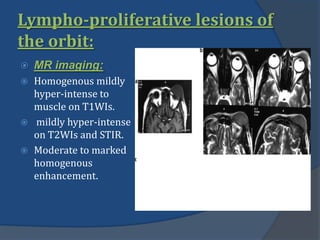
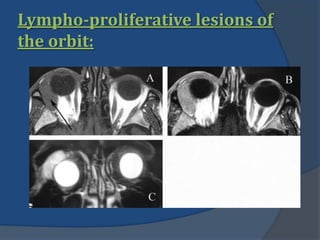
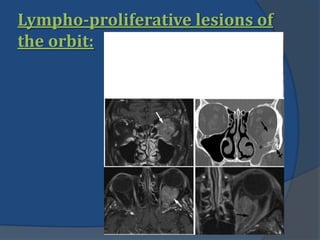
The document discusses several pathologies that can cause proptosis (forward displacement) of the eye including orbital pseudotumor, Graves' ophthalmopathy, optic neuritis, and lymphoproliferative lesions of the orbit. Orbital pseudotumor is a non-granulomatous inflammatory process that can involve any orbital structure. Graves' ophthalmopathy is associated with thyroid dysfunction and causes enlargement of the extraocular muscles. Optic neuritis typically causes enlargement and enhancement of the optic nerve. Lymphoproliferative lesions include benign lymphoid hyperplasia and lymphomas, appearing as enhancing masses or infiltrative lesions.